This post was written by Janelle Weaver, PhD, a freelance writer
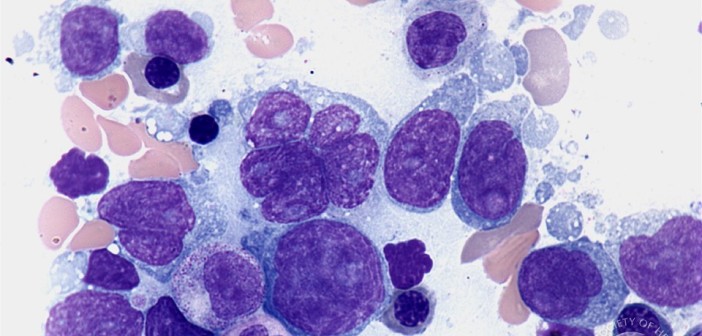
Lymphoma is the most common blood cancer in the United States and is responsible for about 20,000 deaths each year. This type of cancer begins in white blood cells called lymphocytes, which normally play an important role in the immune system by recognizing and responding to pathogens such as bacteria and viruses. To control infections, these cells must multiply in a process that depends on a protein called MALT1. But when inappropriately activated, MALT1 drives the survival of lymphoma cells, underscoring the need to monitor the activity of this protein to develop novel diagnostic tests and facilitate drug discovery.
Sanford-Burnham researchers have made substantial progress toward this goal by developing activity-based probes that selectively label the active form of MALT1. As reported recently in Chemistry & Biology, the probes allow researchers to trace MALT1’s activity profile and study the function of this important protein, paving the way for the development of next-generation diagnostic tools and therapies.
“MALT1 represents a promising therapeutic target because it is a key regulator of immune-cell activation and it promotes the survival of distinct aggressive lymphomas. But until now, a reliable tool to detect this protein in lymphoma cells was missing,” said senior study author Guy Salvesen, PhD, dean of the Sanford-Burnham Graduate School of Biomedical Sciences and professor in our NCI-designated Cancer Center. “The activity-based probes we developed represent powerful chemical tools to measure cellular MALT1 activation, determine the efficacy of small-molecule inhibitors, and classify lymphomas based on MALT1 activity status. In the end, this could translate into more-accurate diagnostic tests that greatly facilitate therapeutic decisions.”
Promising probes To develop the new probes, Salvesen teamed up with Matthew Bogyo, PhD, professor of pathology and of microbiology and immunology at the Stanford School of Medicine, and Marcin Drag, PhD, associate professor of bioorganic chemistry at the Wroclaw University of Technology in Poland. The probes consist of a peptide sequence that determines enzyme selectivity, an electrophilic warhead that irreversibly inhibits the targeted enzyme, and a label that allows detection and activity monitoring. The researchers demonstrated that the imaging probes specifically bind to the active site on MALT1 and can differentiate between active and inactive MALT1 in a lymphoma cell line. The new approach is sensitive enough to detect small but potentially important effects involving MALT1 activity.
In an independent study also published in Chemistry & Biology, Daniel Krappmann of the German Research Center for Environmental Health and his team also developed activity-based probes to detect active MALT1 in tumor cell lines and biopsies. The researchers demonstrated that these probes could help to foster drug discovery by determining the efficacy of MALT1 inhibitors.
Moving forward, the activity-based probes may shed new light on the role of MALT1 in lymphoma as well as autoimmune diseases such as multiple sclerosis, which occurs when the body’s own immune cells attack the nervous system and cause symptoms such as painful muscle spasms, loss of vision, and trouble chewing and swallowing. MALT1 activity is enhanced in immune cells in a mouse model of multiple sclerosis, and MALT1 deficiency protects mice from this disease, suggesting that MALT1 inhibition may be used to treat autoimmune diseases in humans.
“Activity-based probes will help us develop diagnostic tests for lymphomas and inflammatory diseases that are dependent on inappropriate activation of MALT1, allowing for more directed therapy against this protein,” Salvesen said. “Moreover, the tool could be used to monitor patient responses to pharmacological inhibitors that target the MALT1 pathway, helping clinicians fine-tune their treatment strategy to increase the likelihood of positive patient outcomes.”