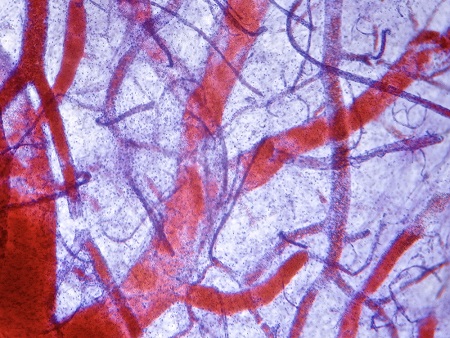
We like to think blood vessels are solid, like a brand-new garden hose—nothing leaks in or out. But sometimes vessels lose integrity, a condition called vascular permeability. This can be a big problem, particularly in cancer, allowing tumor cells to get into the bloodstream and travel throughout the body.
Researchers in the Komatsu laboratory at SBP’s Lake Nona campus in Orlando, Fla. have been studying permeability for some time, focusing on a protein called RRAS that’s known to stabilize blood vessels. Recently, Carole Perrot, PhD, a postdoc in the lab, was the first author on a paper in The FASEB Journal that showed RRAS is regulated by a molecule called cAMP. How that regulation played out was a big surprise.
“I thought cAMP would increase RRAS expression,” says Perrot, “but it was completely the opposite.”
Perrot’s expectations were built on previous research, which showed that cAMP reduces permeability. However, those studies weren’t long enough to fully understand what was happening inside the cells. Because cAMP is a signaling molecule that turns on several genes, it can take time before the results become apparent.
“When cAMP is activated in the short term, it’s beneficial for vasculature,” says Perrot. “But if you activate the pathway for the long term, more than 48 or 72 hours, it does the opposite. You need more time to see which genes are triggered after the initial activation.”
Over time, cAMP downregulates RRAS and destabilizes blood vessel cells’ contacts, making them more permeable. This fits with other evidence, which has shown that key proteins in the cAMP pathway are upregulated in tumor blood vessels.
The ultimate goal is to better modulate RRAS and restore blood vessel functionality. Perrot and colleagues are continuing to identify the various pieces of this puzzle, and the next step will be to find the upstream molecules that trigger cAMP expression. This ongoing research could eventually provide new ways to combat metastasis.
“If you suppress blood vessel leakage, it makes it easier for drugs to reach into the tumor during cancer therapy. Also, there is less opportunity for cancer cells to get into the blood vessels and disseminate throughout the body,” says Perrot. “If you restore RRAS expression in tumors, you normalize the vascular networks and potentially limit tumor progression.”