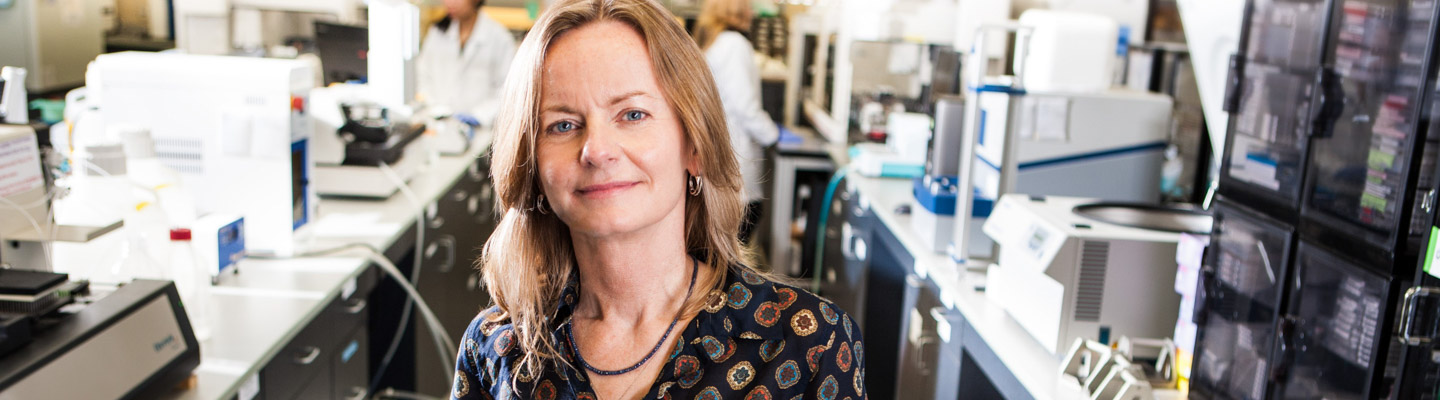
When Joana Borlido, PhD, got the call that she won the inaugural Fishman Fund Fellowship late on a Friday afternoon, she called her parents, who had been waiting up past midnight in her native Portugal to find out if she had won the prestigious two-year postdoctoral fellowship along with a $5,000 career-development cash grant.
After all, her mother, a science teacher, had inspired Borlido to go into science by bringing home props of human body parts and subscribing to an immunology comic series. Yes, those biology cartoons do exist.
On September 15, the Fishman Fund ceremony honored Borlido and Fishman Fund Career Development recipients Bernhard Lechtenberg, PhD, and Jia (Zack) Shen, PhD
In celebration of SBP’s 40th anniversary, the significance of the Fishman Fund has been elevated with the addition of a two-year postdoctoral award called the Fishman Fund Fellowship. The Fishman Fund Fellowship is an incredible award that not only compensates exceptional postdocs at a higher income level than a typical fellowship, but also comes with a one-time $5,000 flexible career-development award, which they can use to further their professional endeavors. The established Fishman Fund Career Development awards of $10,000 will continue to be awarded as well.
Since the Fishman Fund’s inception in 2001, the Fishman Fund has grown from $1,500 cash awards. It was first established by Horowitz and Mary Bradley in honor of founders Dr. William and Lillian Fishman. In 2010, Jeanne Jones became the co-founder designee.
During the ceremony, Fishman Fund co-founder Reena Horowitz discussed the importance of supporting “the next generation of biomedical trailblazers.” She also said that the “Fishmans believed passionately in cultivating early-stage scientific talent. They knew that young investigators must focus intently on honing research skills and gaining professional experience.” Horowitz also took a moment to honor friends and supporters who have passed: Mary Bradley, Erna Viterbi, Pauline Foster, and Conrad Prebys.
Nina Fishman, daughter of SBP founders Dr. William and Lillian Fishman, read from a speech her father gave at the Institute. He said, “Each is encouraged to develop original ideas, which can be tested experimentally and subsequently qualify for grant support. Together we have the ‘critical mass’ of intellectuals and skills to accelerate progress in sciences.” She added that the Institute has demonstrated that a “relatively small but highly focused group can provide a nucleus where the whole is greater than the sum of its parts.”
Past winner Petrus de Jong, MD, PhD, shared how the Fishman Fund has boosted his career. With the grant, de Jong attended a drug delivery systems symposium with biotech entrepreneurs, participated in a research symposium in pancreatic cancer and received tailored career advice from senior scientists. “These events have been crucial for my personal career development, which would not have been possible without the Fishman Fund Award,” he said.
Fishman Fund Fellowship Awardee:
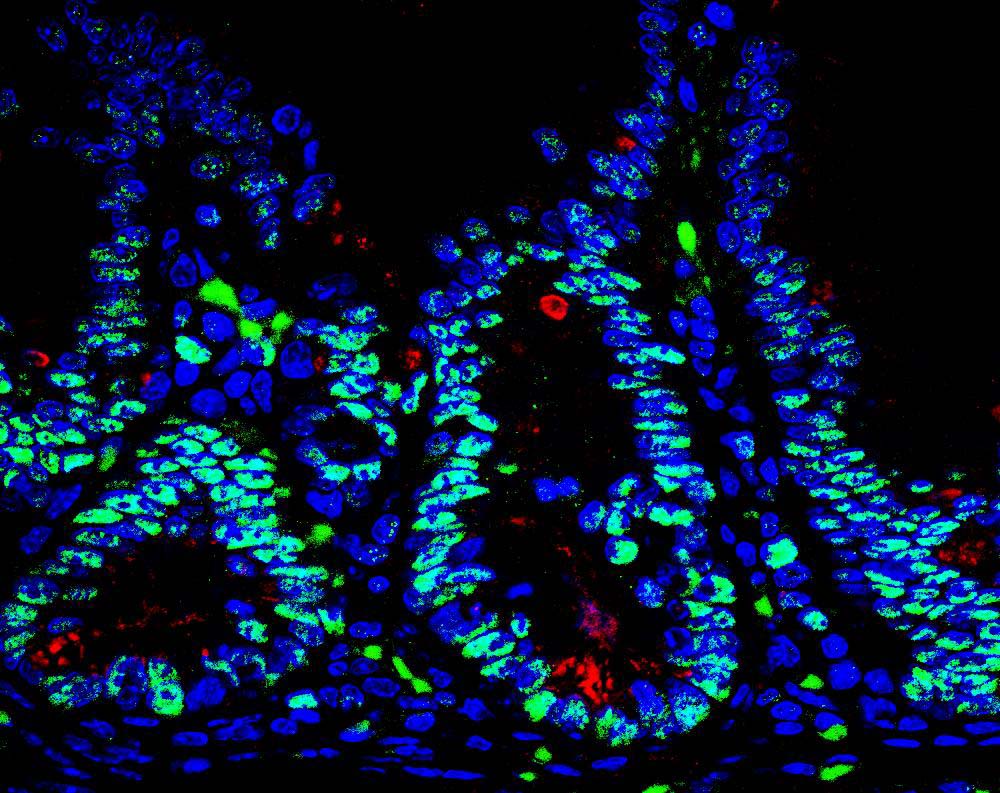
Joana Borlido, PhD, explores the mechanisms through which the channels that connect the cell nucleus (where the genome is stored) affect the immune system. She works in the laboratory of Maximiliano D’Angelo, PhDHer work will help elucidate the molecular basis for the onset and development of leukemia.
She completed her PhD in Oncology at the University of Cambridge in the U.K. and her BS in Biology at the University of Porto in Portugal.
If Borlido is not in the lab, she can usually be found playing foosball, which she admits she would play during all her free time if she could.
Fishman Fund Career Development Recipients:
Bernhard Lechtenberg, PhD, studies cellular signaling networks in normal human physiology and diseases in the laboratory of Stefan Riedl, PhDLechtenberg uses protein X-ray crystallography to study diseases such as cancer and ALS (Lou Gehrig’s disease). He received his BS and MS from the University of Luebeck in Germany and his PhD from the University of Cambridge in the U.K.
In his spare time, he and his wife Anne Hempel, also a SBP postdoc, participate in Ragnar Relay races, in which a team runs nonstop day and night to complete a course of almost 200 miles.
Jia (Zack) Shen, PhD, develops functional screens of for drugs that inhibit ubiquitin ligases (enzymes that tag proteins with a small protein called ubiquitin). Such drugs, alone and in combination with current chemotherapies, are considered important advances in the therapy of breast cancer patients. Shen works in the laboratory of Charles Spruck, PhD, and received his BS from Zhejiang Sci-Tech University and his PhD from the Chinese Academy of Sciences.
He and his wife love taking their 6-month-old daughter Olivia for walks in San Diego. Shen also plays soccer twice a week with a team at the Salk Institute.
With the generous support of the Fishman Fund, this stellar group of postdocs will benefit tremendously from well-earned rewards for their hard work and vision for “Science Benefiting Patients.”