For two weeks this summer, eight rising juniors at The Preuss School at UC San Diego came to Sanford Burnham Prebys Medical Discovery Institute (SBP) each day to try their hands at laboratory techniques ranging from microinjection to dissection to real-time microscopy. This was the first time most had ever been in a research lab, and the experience opened their eyes to what science is like and the range of opportunities that studying biology can open.
“What we did here was much closer to real science than our labs in school,” said participant Bao Lam. “We got to try the methods that scientists use every day, and collect real data and draw conclusions from it.”
This exposure to scientific research is especially significant for students from The Preuss School, which serves low-income students who strive to become the first in their families to graduate from college.
The students rotated through four labs, where they worked with
- tiny soil roundworms, used to study aging
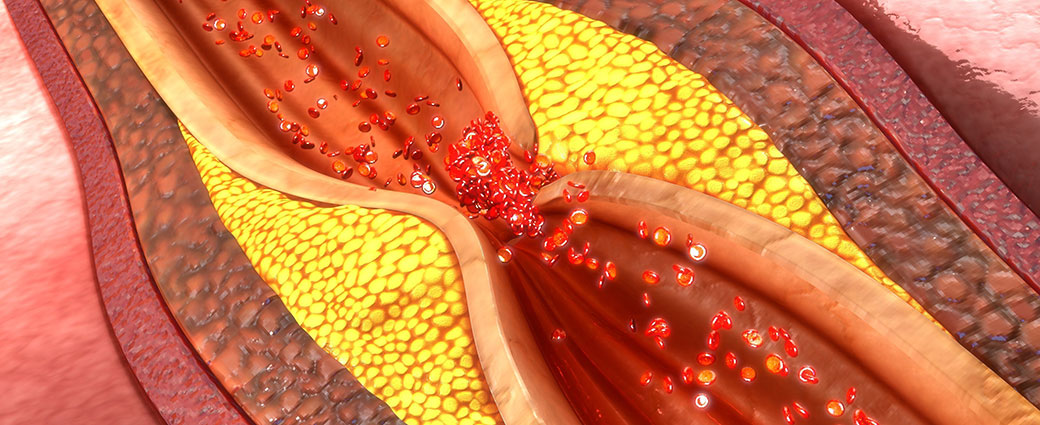
- fruit flies, used to study heart disease and obesity,
- zebrafish, used in research towards cellular reprogramming treatments for diabetes, and
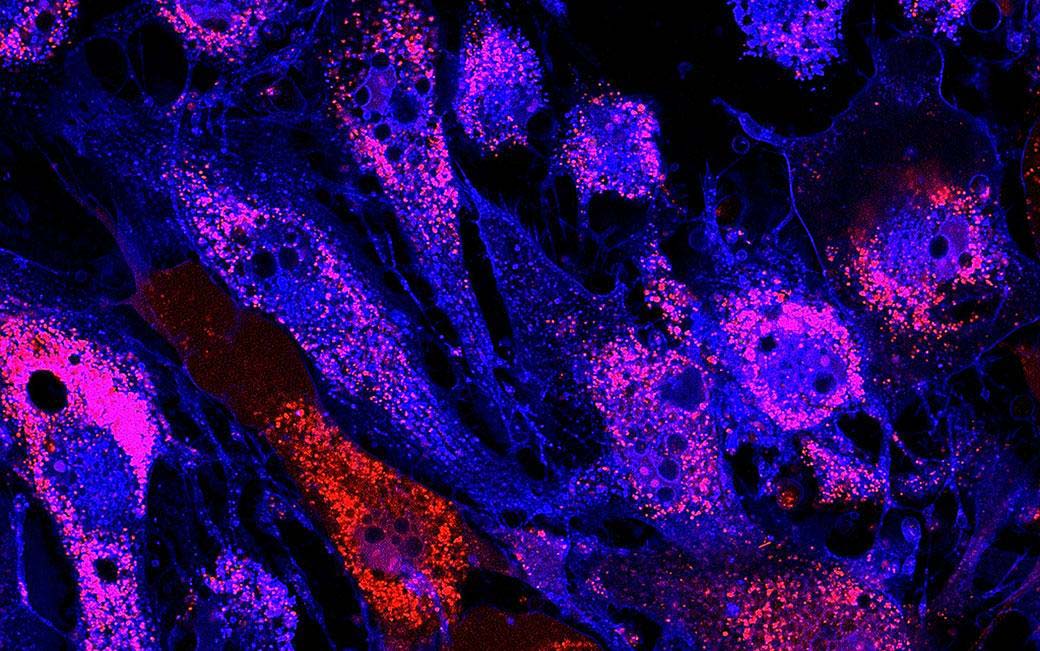
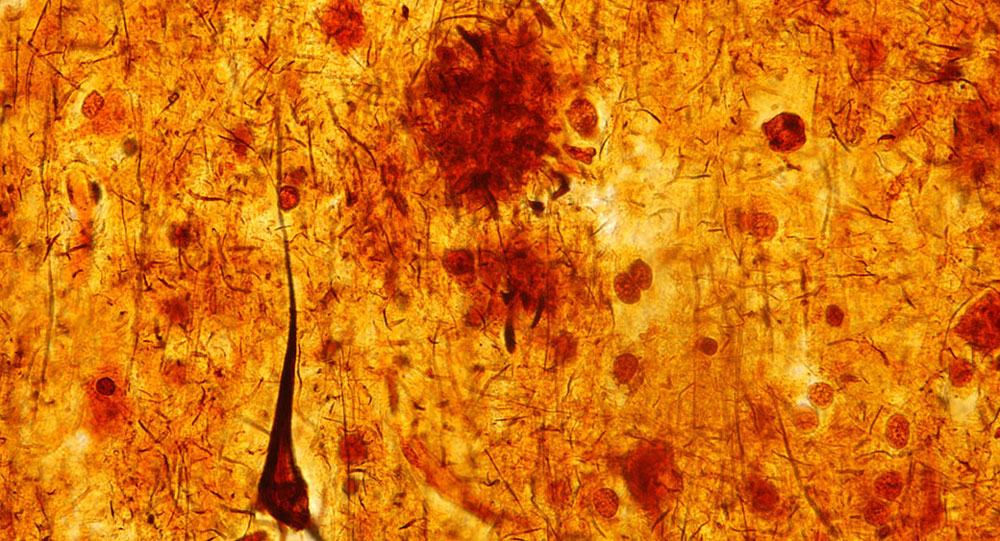
- mouse cells, used to study regulation of gene activity.
“I would definitely work in a lab again,” said Jennifer Vazquez-Gonzalez. “I gained an appreciation for how research can make a difference—the goal is to help patients.”
In the course of their rotations, the students interacted with many researchers, which helped give them a more realistic understanding of what scientists are like.
“I used to think all scientists were bald and boring,” said America Sanchez Radilla. “But the people we worked with were young and diverse and fun to be around.”
The group was also exposed to scientific career paths other than laboratory research. The program included a visit to the campus of Illumina, a leading producer of genetic sequencing equipment, and a panel discussion where they heard from professionals who support research in a variety of ways.
Those who especially enjoyed their time at SBP may come back next year for a more in-depth experience—the Institute also organizes a six-week program where students carry out their own project.
The program is made possible by philanthropists Peggy and Peter Preuss and Debby and Wain Fishburn.