Phenomena or Process: Innate Immunity
Kevin Tharp studies the interplay between mitochondrial metabolism and the physical properties of the tumor microenvironment, using genetically engineered mouse models and bioengineered human tumor models to define the mitochondrial programming unique to cancer cells in the tumor microenvironment.
His goal is to develop new therapies that block the metabolic adaptations that cancer cells use to metastasize, a major cause of cancer-associated mortality.
“I study how cells make decisions about their metabolic programming, which I expect will enable us to develop new therapeutics against metastatic tumor cells.”
Tharp previously worked as a postdoctoral scholar in the Center for Bioengineering & Tissue Regeneration at UCSF Health.
He completed his PhD in metabolic biology at UC Berkeley and his Bachelor of Science degree in biochemistry and molecular biology at UC Santa Cruz, where he graduated with honors and the Dean’s Award in Chemistry.
He has received meritorious funding awards from the Sandler Foundation and the National Institutes of Health/National Cancer Institute for his postdoctoral research.
Phenomena or Processes
Actin Cytoskeleton, Adipocyte Differentiation, Aging, Apoptosis and Cell Death, Cancer Biology, Cancer Metabolism, Cancer-Associated Glycans, Cell Adhesion and Migration, Cell Differentiation, Cell Signaling, Combinatorial Therapies, Damage-Associated Molecular Patterns, Extracellular Matrix, Glycosylation, Inflammation, Innate Immunity, Integrins, Metabolic Networks, Mitochondrial Biology, Organic/Synthetic/Medicinal Chemistry, Tumor Microenvironment, Tumorigenesis
Anatomical Systems and Sites
Adipose Tissue, General Cell Biology, Immune System and Inflammation, Mammary Gland, Vasculature
Research Models
C. elegans, Human, Human Cell Lines, Mouse, Mouse Cell Lines, Primary Cells
 Nov 4, 2024
Nov 4, 2024The implastic nature of plastic culture
Nov 4, 2024There is an art (and science) to creating cell culture models that reflect the complexities of disease.
 Oct 31, 2024
Oct 31, 2024Raising awareness of breast cancer research at Sanford Burnham Prebys
Oct 31, 2024The October Science Connect Series event was themed around Breast Cancer Awareness Month.
 Jun 4, 2024
Jun 4, 2024How tumor stiffness alters immune cell behavior to escape destruction
Jun 4, 2024Immunotherapy is based on harnessing a person’s own immune system to attack cancer cells. However, patients with certain tumors do…
 Mar 25, 2024
Mar 25, 2024Seminar Series: extrachromosomal DNA and the metabolic circuits of cancer immune suppression
Mar 25, 2024The ongoing Sanford Burnham Prebys seminar series will feature a pair of speakers on March 27, from noon to 1p.m.,…
 Dec 18, 2023
Dec 18, 2023When tumors manipulate their mitochondria, Kevin Tharp will be there to stop them
Dec 18, 2023Newly arrived at Sanford Burnham Prebys, Tharp will look at how cellular mechanics can be leveraged to create more effective…
 Nov 2, 2023
Nov 2, 2023La Jolla’s Sanford Burnham Prebys adding six scientists in hopes of launching new era of collaboration
Nov 2, 2023The newcomers, brought in with help from a $70 million donation, are versed in different technologies that can be applied…
Xueqin (Sherine) Sun seeks to better understand the genetic and epigenetic underpinnings of cancers, using genome editing technologies, animal and patient-derived models, and other tools to develop more effective cancer therapies.
“My lab is interested in studying how DNA or the machinery that interprets it leads to the transformation of normal cells into cancerous cells and concurrently, their specific vulnerabilities. Identifying these intrinsic vulnerabilities and targeting them properly is profoundly important to developing effective cancer therapies.”
Another aspect of Sun’s work is understanding how cancer cells and tumors change their circumstances and environment to improve survival, including hiding from or repressing the immune system.
“Changes to DNA itself and the way how DNA is interpreted by cells can transform normal cells into cancer cells. And transformed cells propagate by enhancing the misinterpreted DNA information, which in turn becomes the Achilles’ heel of cancer cells. Our goal is to find out how DNA information is misinterpreted in different ways and how to correct it to halt cancer.”
At Sanford Burnham Prebys, Sun and colleagues will employ a host of leading-edge tools and approaches, including functional genomics, artificial intelligence, structural biology, large-scale drug screening, and advanced imaging/spatial technologies.
Sun conducted her postdoctoral fellowship at Cold Spring Harbor Laboratory under the guidance of Alea Mills, PhD, a professor at the National Cancer Institute-designated cancer center at Cold Spring Harbor.
She received her PhD from Wuhan University in China.
Related Disease
Aging-Related Diseases, Brain Cancer, Cancer, Childhood Diseases, Immune Disorders, Inflammatory/Autoimmune Disease, Leukemia/Lymphoma
Phenomena or Processes
Adapter Proteins, Adult/Multipotent Stem Cells, Aging, Angiogenesis, Apoptosis and Cell Death, Bcl-2 Family, Cancer Biology, Cancer Epigenetics, Cell Adhesion and Migration, Cell Biology, Cell Cycle Progression, Cell Differentiation, Cell Motility, Cell Proliferation, Cell Signaling, Cell Surface Receptors, Cellular Senescence, Chromosome Dynamics, Combinatorial Therapies, Cytokines, Development and Differentiation, Disease Therapies, DNA Damage Checkpoint Function, Embryonic/Pluripotent Stem Cells, Epigenetics, Gene Regulation, Genomic Instability, Growth Factors, Hematopoiesis, Host Defense, Host-Pathogen Interactions, Inflammation, Innate Immunity, Kinase Inhibitors, Metastasis, Neurogenesis, Oncogenes, Phosphorylation, Posttranslational Modification, Receptor Tyrosine Kinases, Serine/Threonine Kinases, Signal Transduction, TNF-Family, Transcription Factors, Transcriptional Regulation, Tumor Microenvironment, Tumorigenesis, Tyrosine Kinases, Ubiquitin, Ubiquitin Protease System and Ubiquitin-like Proteins
Anatomical Systems and Sites
Brain, General Cell Biology, Hematopoietic System, Immune System and Inflammation, Nervous System
Research Models
Bacteria, Cultured Cell Lines, Human Adult/Somatic Stem Cells, Human Cell Lines, Mouse, Mouse Cell Lines, Mouse Embryonic Stem Cells, Mouse Somatic Stem Cells, Primary Cells, Primary Human Cells
Techniques and Technologies
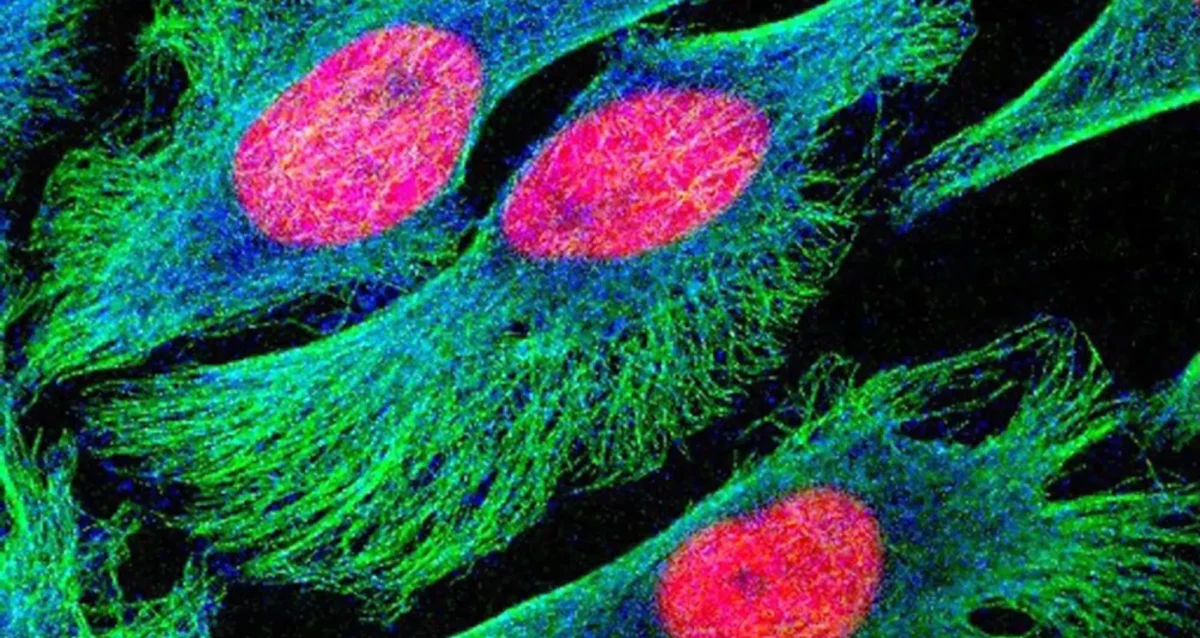
3D Image Analysis, 3D Reconstructions, Biochemistry, Bioinformatics, Cell Biology, Cellular and Molecular Imaging, Chemical Biology, Computational Biology, Confocal Microscopy, Correlative Light and Electron Microscopy, Drug Delivery, Drug Discovery, Drug Efficacy, Electron Microscopy, Fluorescence Microscopy, Fragment-Based Drug Design, Gene Expression, Gene Knockout (Complete and Conditional), Gene Silencing, Genetics, Genomics, High Content Imaging, High-Throughput/Robotic Screening, In vivo Modeling, Live Cell Imaging, Live Imaging, Mass Spectrometry, Microscopy and Imaging, Molecular Biology, Molecular Genetics, Nucleic Acid Synthesis, Protein-Protein Interactions, Protein-Small Molecule Interactions, Proteomics, Rational Drug Design, RNA Interference (RNAi), Scanning Cytometry, Small Molecule Compounds, Transgenic Organisms, Transplantation
We seek to understand why cancer occurs and what is the Achille’s heel of cancer, and to develop effective therapeutic interventions.
The successful treatment of any disease requires a good understanding of the mechanisms at work. Cancer is fundamentally caused by aberrant gene expression, which reflects the misinterpretation of DNA information at both genetic and epigenetic levels. We are interested in uncovering DNA-related alterations that drive cancer-favored transcriptional programs, identifying cancer-specific vulnerabilities, and developing effective therapeutic interventions for cancer treatment.
Xueqin Sun’s Research Report
Precise gene expression (the interpretation of DNA) is essential for almost all biological processes, and understanding gene regulation is one of the most pivotal frontiers in biological research under both health and disease circumstances. Gene expression is mainly regulated at genetic (with changes of DNA sequence) and epigenetic (without changing DNA sequence) levels. And gene dysregulation can lead to various health conditions and diseases, including developmental disorders, aging, and cancer. The overarching goal of Sun Lab is to uncover driving genetic and epigenetic alterations involved in cancer, to understand how developmental pathways and aging process impact cancer progression, and to identify mechanisms of action for developing more effective therapeutic strategies.
We are an interdisciplinary lab particularly focused on the following research directions:
- The EP400 chromatin remodeling complex
The EP400 complex is an evolutionarily conserved SWR1-class ATP-dependent chromatin remodeling complex encompassing ~17 components, with a total molecular mass of ~1.5 mega-dalton. The EP400 complex plays critical roles in diverse cellular processes, including chromosome stability, transcription, DNA recombination, DNA damage repair, embryonic stem cell renewal/development, and oncogenesis. The EP400 complex can incorporate histone variants, such as H2AZ and H3.3, into the genome to regulate gene expression. Our recent work discovers BRD8—one of the core subunits of the EP400 complex—as a unique vulnerability of p53 wildtype glioblastoma (GBM), the most prevalent and devastating type of brain cancer. BRD8-driven EP400 complex highjacks H2AZ at p53 target loci to block p53-mediated transactivation and tumor suppression (Nature, 2023). The bromodomain of BRD8 plays the key role in this process. Bromodomain is a druggable domain as evidenced by a number of successful small molecules targeting diverse bromodomains encoded by the human genome across multiple cancer types. Furthermore, findings from others and us suggest that the EP400 complex is involved in different cancers. Thus, we seek to unravel the roles of the EP400 complex in health and disease, and to better understand how to target the EP400 complex for developing effective therapeutic interventions. - The NuRD chromatin remodeling complex
The NuRD complex is also a highly conserved class of ~ 1 MDa multi-subunit chromatin remodeling complexes that consume energy derived from ATP hydrolysis to remodel the configuration of chromatin to control gene transcription programs, with a primary role in gene silencing. Chromatin remodeling is vital for efficiently framing the cellular response to both intrinsic and extrinsic signals and has enormous implications for determining cellular states. NuRD complex is unique in combining ATP-dependent chromatin remodeling, protein deacetylase activity, and recognition of methylated DNA and histone modifications, and has multifarious roles in chromatin organization, transcription regulation, and genome maintenance; thereby, largely impacts health and disease. The NuRD complex has been in the central stage of brain development studies, and is significantly related to brain disorders/diseases. Interestingly, NuRD complex re-assembles by exchanging the chromatin remodeling subunits CHD3/4/5 to achieve specific regulation of an array of genes required for generating distinct cell types in a highly organized manner, especially over brain development. Amongst the genes encoding NuRD complex components, CHD5 is located in human chromosome 1 short arm (1p36), a region that is frequently hemizygously deleted in diverse cancers. Besides genetic deletion, CHD5 is also often silenced in cancer cells due to epigenetic mechanisms, such as promoter hypermethylation, aberrant expression of other chromatin regulators, and microRNAs-mediated translational repression and/or mRNA instability. Our current work seeks to determine whether and how CHD5-driven NuRD complex is involved in tumorigenesis (In preparation, 2024). We will further understand how NuRD complex is involved in both development and tumorigenesis, and identify mechanism of action to develop rational therapeutic strategies. - Novel genetic and epigenetic underpinnings in GBM
GBM is notorious for being a highly complex and plastic cancer type. However, at the genetic level, GBM harbors a relatively low genetic alteration burden compared to the majority of other cancers from pan-cancer profiling studies. This indicates the largely undocumented epigenetic mechanisms that interplay with genetic alterations and co-reprogram transcriptional networks essential for GBM development. Epigenetic changes are usually reversible by nature, as evidenced by numerous successes in targeting epigenetic regulators using small chemical compounds. As actionable therapeutic targets for GBM have been scarce, we are keen to uncover novel epigenetic pathways underlying gliomagenesis under different genetic backgrounds, which will potentially provide promising therapeutic opportunities for GBM treatment. - Novel GBM mouse models
Despite decades of effort, our knowledge about GBM biology is still very limited. GBM harbors a number of genetic alterations. However, among these recurrent genetic lesions, only several have been implicated in gliomagenesis, with most being undocumented. Moreover, the mechanisms by which these genetic alterations are involved in establishing GBM-favored epigenetic landscapes and transcription programs during GBM progression are still largely elusive. The lack of efficient approach to establish mouse models for investigating gene function in gliomagenesis and the limit of current mouse models to recapitulate clinical GBM features in brain is the prime reason that hinders GBM biological research. To this end, we have developed an engineered neural stem cells (NSCs)-based strategy to rapidly generate highly aggressive GBM with desired genetic lesions (genotypes) in mouse brain. Therefore, we will further optimize this strategy to establish a series of novel mouse models possessing recurrent combinations of genetic alterations (genotypes) in GBM, in order to systematically study whether and how these genetic lesions are involved in gliomagenesis and identify genotype-specific dependencies. - Crosstalk between GBM cells and tumor microenvironment
GBM exhibits highly diffuse and infiltrative nature, which contributes to therapeutic resistance and tumor relapse after surgical removal, resulting in dismal prognosis. A better understanding of gliomagenesis involving not only malignant cells themselves, but also the holistic bidirectional interactions of malignant cells with a variety of proximal and distal cells within the organism, is profound for developing novel effective therapies to improve GBM prognosis. Individual invasive GBM cells intermingle with normal brain cells and often cause relapse in brain areas essential for patient survival. Emerging evidence indicates that glioma cells highjack normal brain cells to thrive, and even transform them. However, how gliomagenesis reshapes ecological composition/landscape in host brain and how brain microenvironment affects gliomagenesis are still largely unclear. By using our novel highly invasive mouse models that recapitulate the multiforme diffuse topographies of GBM in brain, we seek to understand the interactions between GBM cells and brain microenvironment, and identify extrinsic pathways that are essential for GBM progression and migration.
Our lab is focused on both fundamental questions in cancer biology and translation of promising therapeutic strategies.
To achieve these, we work together with many fantastic collaborators to develop and leverage cutting-edge technologies, including but not limited to, high-throughput functional genomics (CRISPR/Cas9 screens, exon tiling scan, targeted mutagenesis, etc.), cell and molecular biology, genomics, epigenomics, proteomics, biochemistry, microscopy (2D/3D, time-lapse, two-photon, light sheet, etc.), automated large-scale drug synthesis/screening, structural biology, single cell and spatial multi-omics, artificial intelligence, and bioinformatics. We also establish novel patient-derived models and novel mouse models to facilitate our research programs. Our ultimate goals are to better understand fundamental genetic and epigenetic apparatuses involved in cancer-specific transcriptional networks, provide more effective therapeutic opportunities, and contribute to shifting the paradigms in cancer treatment and precision medicine.
 Aug 19, 2024
Aug 19, 2024Women in Science event at Sanford Burnham Prebys examines how female faculty members navigate research careers
Aug 19, 2024Topics at the event included work/life balance, caregiving and family obligations, and gender disparities in academic rank at research and…
 Mar 13, 2024
Mar 13, 2024Xueqin Sun seeks to illuminate the underlying causes of cancer
Mar 13, 2024New Sanford Burnham Prebys scientist investigates the mutational powers of cancer cells — and their vulnerabilities
 Dec 19, 2023
Dec 19, 2023Sanford Burnham Prebys continues unprecedented recruitment of early-career scientists
Dec 19, 2023Continuing its rapid and dramatic recruitment of emerging, top-tier researchers, Sanford Burnham Prebys has hired two more highly regarded early-career…
Charles Spruck earned his BS in Biology at UCLA and PhD in Molecular Biology at the University of Southern California. He worked as a postdoctoral fellow at The Scripps Research Institute in La Jolla and was recruited to the Sidney Kimmel Cancer Center in San Diego as an Assistant Professor in 2003. He joined Sanford Burnham Prebys in 2010.
Education and Training
2003: Post-doc, The Scripps Research Institute
1986: PhD, University of Southern California
1995; BS, University of California at Los Angeles
Prestigious Funding Awards / Major Collaborative Grants
NIH/NCI DoD BCRP CBCRP TRDRP
Honors and Recognition
ACS Scholar
Related Disease
Breast Cancer, Cancer, Lung Cancer, Molecular Biology
Phenomena or Processes
Cancer Biology, Cancer Epigenetics, Cell Biology, Cell Cycle Progression, Cell Signaling, Genomic Instability, Innate Immunity, Metastasis, Posttranslational Modification, Proteolytic Pathways
Research Models
Cultured Cell Lines, Human Cell Lines, Mouse, Mouse Cell Lines
Techniques and Technologies
Cell Biology, Drug Discovery, Gene Knockout (Complete and Conditional), In vivo Modeling
“Despite recent advances in treatment, patients with advanced metastatic cancers have few treatment options. Our lab is focused on developing new effective and non-toxic treatments for these patients.”
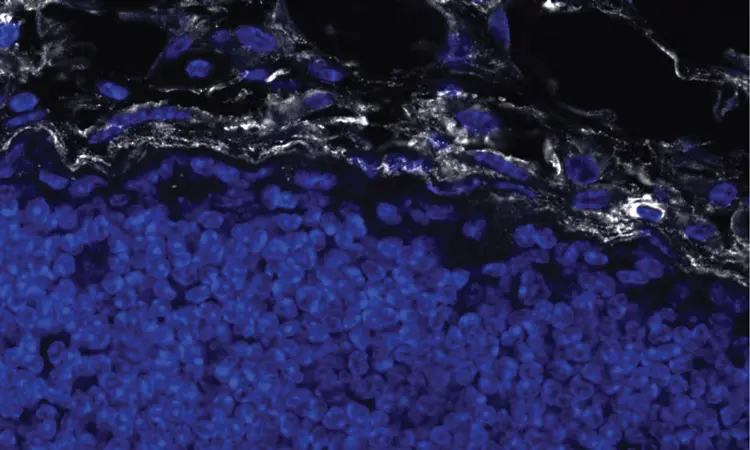
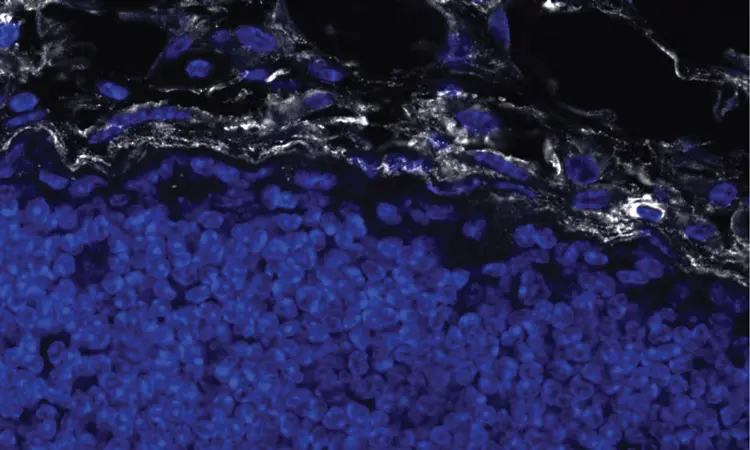
Dr. Spruck’s laboratory is focused on developing new, effective, and non-toxic treatments for patients with advanced cancers. The lab focuses on defining the molecular networks that regulate cancer cell division and drive metastasis progression. Recent studies have focused on viral mimicry as a therapeutic approach in cancer, which involves the activation of dormant endogenous retroviruses and retrotransposons in cancer cells to enhance immunogenicity and the effectiveness of immune checkpoint blockade immunotherapy and DNA damaging therapies. The laboratory utilizes various biochemical and molecular approaches, CRISPR gene editing, and animal models of cancer. An emphasis is on studies of breast, lung, prostate, and brain tumors.
Charles Spruck’s Research Report
Developing viral mimicry therapeutic approaches for cancer: Approximately 45% of the human genome is composed of repetitive elements (REs), including endogenous retroviruses and retrotransposons, that are normally transcriptionally silenced in somatic cells. Recent studies suggest that the transcriptional awakening of ERVs/retrotransposons beyond a threshold level of tolerance in cancer cells induces antiviral responses that can enhance the efficacy of certain therapies, including immunotherapy. We recently discovered a novel epigenetic regulatory pathway, FBXO44/SUV39H1, that is essential for ERV/retrotransposon silencing in cancer cells. Preclinical studies showed that FBXO44/SUV39H1 inactivation induces viral mimicry in cancer cells, leading to increased immunogenicity, decreased tumorigenicity, and enhanced the efficacy of immune checkpoint blockade therapy. We are currently exploring therapeutic approaches to target this pathway, and others like it, to prevent tumor growth and enhance immunotherapy response. We are also exploring the role of reactivated REs in human diseases.
Targeting metastatic tumors: Metastasis is a major cause of mortality in cancer. Through genomic screens and biochemical studies, we are identifying novel molecular pathways that drive cancer cell motility, invasion, and metastasis. Recently, we identified a novel molecular axis, FBXO7/EYA2-SCF(FBXW7), that promotes cancer cell motility and cancer stem cell self-renewal and suppresses cancer cell immunogenicity. Targeting this axis prevented metastasis progression, reduced the cancer stem cell population, and stimulated anti-tumor immune responses in preclinical mouse breast cancer models.
 Apr 24, 2023
Apr 24, 2023Charles Spruck awarded $1.7M to advance “ancient virus” treatment for prostate cancer
Apr 24, 2023The approach uses ancient viruses, embedded in our genomes, to trick the body into thinking it has an infection. With…
 Jun 30, 2022
Jun 30, 2022Three Sanford Burnham Prebys faculty receive promotions
Jun 30, 2022The promoted faculty, all from the Institute’s NCI-designated Cancer Center, include Ani Deshpande, PhD, Brooke Emerling, PhD and Charles Spruck,…
 Mar 15, 2022
Mar 15, 2022Tricking the body to treat breast cancer
Mar 15, 2022With the help of two new grants from the National Institutes of Health totaling more than $4.4 million, Charles Spruck,…
 Nov 3, 2021
Nov 3, 2021Boosting immunotherapy in aggressive brain cancer
Nov 3, 2021Institute have collaborated the University of Pittsburgh Cancer Institute to reveal a new approach to enhance the effects of immunotherapy in…
 Feb 11, 2021
Feb 11, 2021Mining “junk DNA” reveals a new way to kill cancer cells
Feb 11, 2021Scientists unearth a previously unknown vulnerability for cancer and a promising drug candidate that leverages the approach Scientists at Sanford…
 Oct 20, 2016
Oct 20, 2016Hearst Foundation’s new fellowship funds innovative research to fight breast cancer
Oct 20, 2016Mark Goldberg, PhD, is working on a potential way to turn cancer stem cells into harmless cells. He and his…
“Cancer is one the main causes of death in the US. Our research is focused on understanding how we can harness the power of our immune system to attack and kill cancer cells and cure patients. I chose to join Sanford Burnham Prebys because of their collaborative research culture and state-of-the- art core facilities. I believe that teamwork is the foundation of scientific breakthroughs, and the Institute provides a perfect supportive and friendly environment to achieve this.”
Originally from the Netherlands, Kelly received her BS and MS from Utrecht University, and performed her PhD studies at the Netherlands Cancer Institute in Amsterdam working with Prof. Karin de Visser studying the role of the immune system in the metastatic spread of breast cancer. For her postdoctoral training, Kelly joined the lab of Prof. Max Krummel at the University of California San Francisco to study how tumor-associated myeloid cells affect anti-tumor T cell responses. Kelly is currently setting up her independent research team at Sanford Burnham Prebys.
Education
2016-2023: Postdoctoral Training, University of California San Francisco (Mentor: Prof. Max Krummel, focus on immune evasive cancer)
2017: PhD, Netherlands Cancer Institute Amsterdam/ Leiden University (Mentor: Prof. Karin de Visser, focus on role immune system in breast cancer metastasis, 2011-2016)
2011: MS, Biomedical Sciences, Utrecht University, Netherlands
2008: BS, Biology, Utrecht University, Netherlands
Honors and Recognition
2022: Selected Attendee for SITC Women in Cancer Immunotherapy Network (WIN) Leadership Institute
2022: Selected Attendee for Arthur and Sandra Irving Cancer Immunology Symposium
2022: Ray Owen Poster Award for Outstanding Poster Presentation at 60th Midwinter Conference for Immunologists at Asilomar (sponsored by AAI)
2020-2022: Parker Scholar Award awarded by the Parker Institute for Cancer Immunotherapy (PICI)
2018: Honorable Mention of poster presentation at UCSF/UCB/UCM Immunology Retreat
2018: Poster presentation ‘Excellence in Research Award’ awarded by the National Philanthropic Trust
2017-2019: NWO Rubicon postdoctoral fellowship awarded by the Netherlands Organization for Scientific Research (NWO)
2015: Best presentation award at the annual Tumor Cell Biology meeting of the Dutch Cancer Society (KWF)
2014: Travel scholarship awarded by the Dutch Foundation for Pharmacological Sciences (NSFW)
2010: Master scholarship awarded by the Dutch Cancer Society (KWF)
Memberships
2022-present: Society for Immunotherapy of Cancer (SITC)
2020-present: Parker Institute for Cancer Immunotherapy (PICI)
2012-present: American Association for Cancer Research (AACR)
Related Disease
Breast Cancer, Cancer Biology, Immune Disorders, Inflammation, Innate Immunity, Metastasis, Skin Cancer and Melanoma, Tumor Microenvironment, Tumorigenesis
Phenomena or Processes
Adaptive Immunity, Innate Immunity
Research Models
Mouse, Primary Cells
Techniques and Technologies
Cellular and Molecular Imaging
The Kersten lab studies the interactions between the immune system and cancer.
We are fascinated by the crosstalk between the immune system and cancer. Our goal is to understand how cancer cells hijack the normal physiology and function of immune cells to support tumor growth and evade destruction by the immune system.
Kelly Kersten’s Research Report
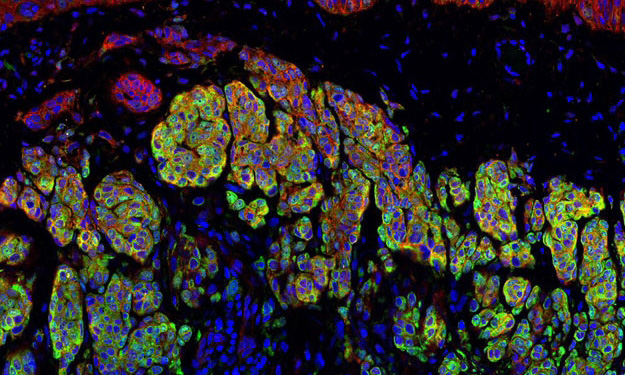
Cancer immunotherapy, harnessing a patient’s immune system to fight cancer, has revolutionized the way we treat cancer. However, a large proportion of patients do not respond to this type of therapy, and we do not fully understand why. In the Kersten lab, we study how different immune cells affect anti-tumor immunity with the ultimate goal to improve therapies to fight cancer. Research in our lab is focused on understanding how interactions between different immune cells in the tumor microenvironment, specifically macrophages and T cells, affect anti-tumor immunity and responsiveness to immunotherapy. Why do T cells become dysfunctional and exhausted? How do exhausted T cells modulate the composition of immune cells in tumors? And how do macrophages shut down anti-tumor T cells? Our research aims to define the molecular mechanisms that regulate these reciprocal signals to design novel anti-cancer therapies. How immune cells function is highly context-dependent. Upon infiltration in the tumor microenvironment, immune cells face extremely harsh conditions characterized by nutrient deprivation, hypoxia and metabolic challenges resulting in their failure to function properly. We study how different environmental factors impact immune cell phenotype and function, with the goal to optimize their cancer-killing properties.
 May 2, 2025
May 2, 2025Kelly Kersten awarded Melanoma Research Alliance grant to support research on melanoma immunotherapy
May 2, 2025The newly created award is part of the alliance’s $9.3 million commitment to melanoma research funding in 2025.
 Oct 31, 2024
Oct 31, 2024Raising awareness of breast cancer research at Sanford Burnham Prebys
Oct 31, 2024The October Science Connect Series event was themed around Breast Cancer Awareness Month.
 Jun 4, 2024
Jun 4, 2024How tumor stiffness alters immune cell behavior to escape destruction
Jun 4, 2024Immunotherapy is based on harnessing a person’s own immune system to attack cancer cells. However, patients with certain tumors do…
 Feb 7, 2024
Feb 7, 2024Speaking of International Day of Women and Girls in Science
Feb 7, 2024Designated by the United Nations, the 9th International Day of Women and Girls in Science is Sunday, February 11, preceded…
 Jan 17, 2024
Jan 17, 2024When T cells and macrophages talk, Kelly Kersten listens
Jan 17, 2024New Sanford Burnham Prebys scientist probes and parses the complex microenvironment of cancer looking for new ways to boost immunotherapies
 Nov 2, 2023
Nov 2, 2023La Jolla’s Sanford Burnham Prebys adding six scientists in hopes of launching new era of collaboration
Nov 2, 2023The newcomers, brought in with help from a $70 million donation, are versed in different technologies that can be applied…
Dr. Blaho began her research career focused on how bioactive lipids contribute to the innate immune response against bacterial infection, characterizing roles for eicosanoids in the generation and resolution of Lyme arthritis pathology. The wild diversity of lipid species led Dr. Blaho to Weill Cornell Medical College in New York City to pursue postdoctoral training in the field of sphingolipids, particularly sphingosine 1-phosphate (S1P), and its receptors. Advancing to Instructor at Weill Cornell and later, Research Assistant Professor at Sanford Burnham Prebys, Dr. Blaho continued her research in lipid chaperones and receptor signaling, with an emphasis on cell-type differential effects on hematopoiesis and immunity in response to cell stressors. In August of 2019, Dr. Blaho joined the faculty at the Institute as an Assistant Professor in the Immunity and Pathogenesis program.
“The immune system has the power to protect us from invading pathogens and cancer or to initiate a ‘self-destruct’ sequence that consumes us with inflammation and autoimmunity. It is fascinating to me that a simple ubiquitous fat molecule like S1P can control the birth and destiny of immune cells.”
Education
2014-2016: Instructor, Weill Cornell Medicine, Pathology and Laboratory Medicine and Neuroscience
2009-2014: Post-doctoral training, Weill Cornell Medicine, Pathology and Laboratory Medicine
2007-2009: Post-doctoral training, University of Missouri, Columbia, Veterinary Pathobiology
2007: PhD, University of Missouri, Columbia, Molecular Microbiology and Immunology – BS
Funding Awards and Collaborative Grants
National Heart, Lung, and Blood Institute R01
American Heart Association Scientist Development Grant
2014-15: Leon Levy Neuroscience Foundation Grant
2015: Foundation LeDucq SphingoNet Young Investigator Grant
2009-12: National Cancer Institute Individual Ruth L. Kirschstein Post-doctoral Fellowship
Honors and Recognition
2017: British Journal of Pharmacology Lecture: FASEB Summer Research Conference on Lysophospholipids and Related Mediators–from bench to clinic.
2014: Leon Levy Foundation Neuroscience Fellow
2010: Keystone Scholarship, Bioactive Lipids: Biochemistry and Diseases
2008: Keystone Scholarship, Eicosanoids and Other Mediators of Chronic Inflammation
2007: Young Investigator Award in Inflammation, Eicosanoid Research Foundation
2004: National Academy of Sciences Christine Mirzayan Policy Fellow, Institute of Medicine Board on Health Sciences Policy
Related Disease
Biochemistry, Immune Disorders, Inflammatory/Autoimmune Disease, Leukemia/Lymphoma, Molecular Biology, Multiple Sclerosis
Phenomena or Processes
Adaptive Immunity, Apoptosis and Cell Death, Cell Signaling, G-Protein Coupled Receptors, Hematopoiesis, Inflammation, Innate Immunity
Anatomical Systems and Sites
Hematopoietic System, Immune System and Inflammation, Vasculature
Research Models
Human Adult/Somatic Stem Cells, Mouse, Mouse Somatic Stem Cells, Primary Cells
Techniques and Technologies
Cell Biology, Cellular and Molecular Imaging, Confocal Microscopy, Fluorescence Microscopy, Gene Expression, Lipid Bilayers, Mass Spectrometry
The lipid sphingosine 1 phosphate (S1P) is found in high levels in the blood and lymph and is primarily carried by the protein ApoM, found on HDL. S1P can affect the cardiovascular, nervous, and immune systems via interaction with cell surface-expressed receptors, S1P1-5. My work is determining how changing S1P carrier or receptor expression and signaling can affect cells of the immune system, particularly in the bone marrow, and how this alters their ability to respond to stress or infection.
 Dec 22, 2021
Dec 22, 2021A strange research ecosystem: Discussing Lyme disease with Victoria Blaho
Dec 22, 2021As an infectious disease immunologist studying Lyme disease, Victoria Blaho is one of a rare breed. Sanford Burnham Prebys assistant…
 Apr 22, 2021
Apr 22, 2021Victoria Blaho receives prestigious Lina M. Obeid Award
Apr 22, 2021The award honors Obeid, a pioneer in the field of sphingolipids and a fierce advocate for women in science. Victoria…