To find new treatments for schizophrenia and bipolar disorder, scientists and drug companies are turning to stem cells.
Under a $15.4 million contract from the National Institute of Mental Health, Rusty Gage of the Salk Institute and Hongjun Song of Johns Hopkins University will lead a program to grow cells from patient volunteers for screening potential drugs.
Skin cells from the patients will be converted into stem cells and then into brain cells, providing a "disease in a dish" model of abnormal functioning. Potential drugs will be tested on the brain cells to examine their effectiveness in restoring normal function.
Two drug companies, Janssen Research & Development and Cellular Dynamics International, are also taking part in the program. They can use their results for their own drug development programs.
NIMH introduced this model in 2013 to encourage collaboration between researchers and drugs companies that can benefit everyone. These agreements are especially important for difficult diseases, such as Alzheimer's. A reliable body of research increases the odds that companies can develop effective drugs.
Other academic partners are Anne Bang of Sanford Burnham Prebys Medical Discovery Institute; and stem cell researcher Sue O’Shea of the University of Michigan.
The drug companies will help by contributing their own insights into how to most effectively translate the research findings into commercial programs, Gage said.
"One of the things that's exciting for San Diego is working with Janssen, which has a big footprint here," he said.
Moreover, other drug companies will be free to use this "pre-competitive" research for their own proprietary commercial programs, Gage said.
Psychiatric illnesses such as bipolar disorder and schizophrenia fall under the category of difficult-to-treat diseases. Unlike Alzheimer's, effective treatments exist. However, not all benefit, and these intractable cases present a severe challenge, causing distress to those affected and those close to them.
Bipolar disorder affects 2.6 percent of adult Americans, according to NIMH, and schizophrenia affects 1.1 percent. Treatments address symptoms, but generally don't address the underlying causes, which are largely unknown.
Meaningful results
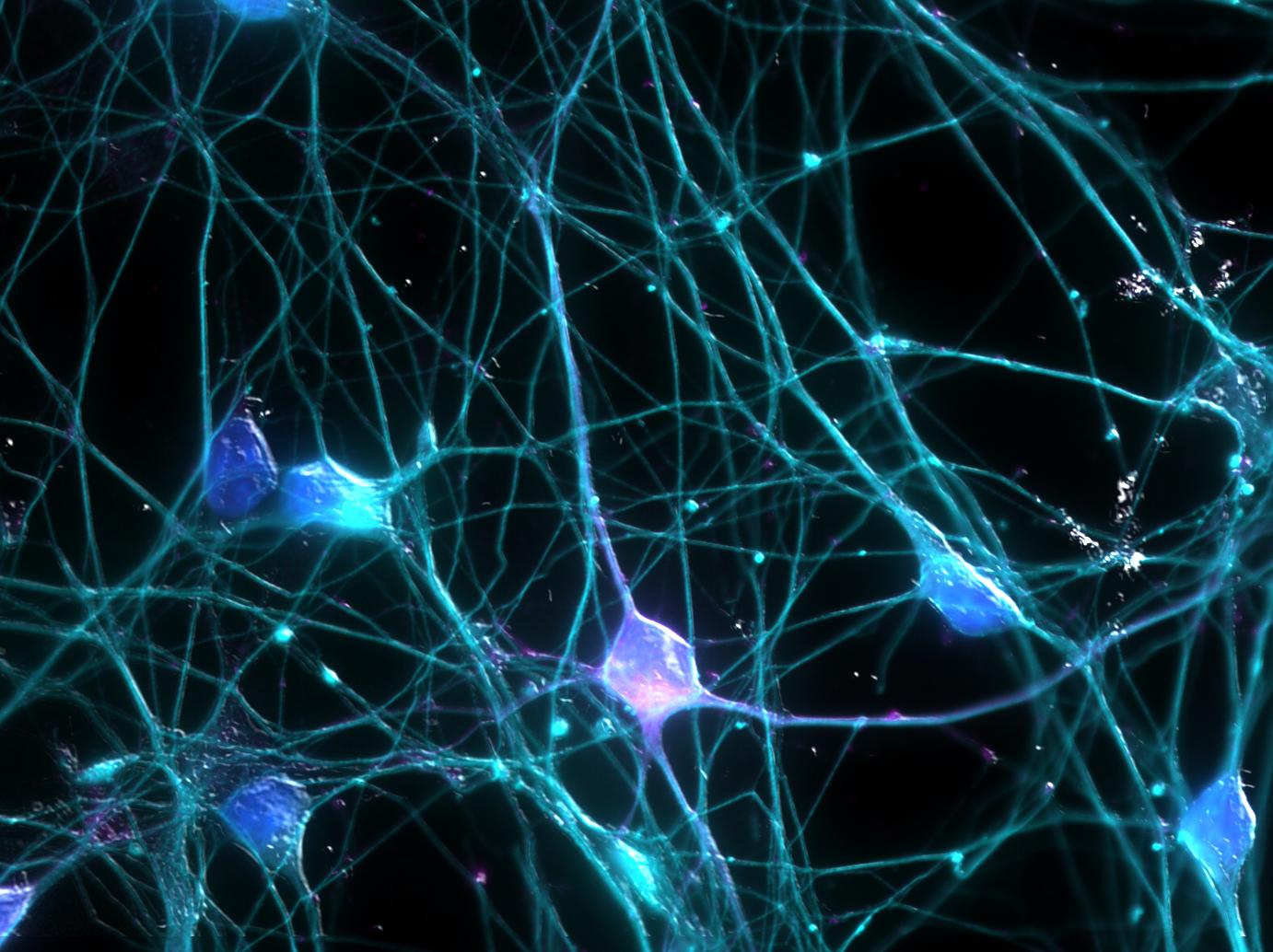
By using stem cells, scientists hope to probe deeper into brain functions to find these causes. They're using artificial embryonic stem cells, which can be converted into nearly any cell type, including neurons and other brain cells.
These stem cells, called induced pluripotent stem cells, provide a way of creating human brain cells safely and ethically from patients in a way not possible before.
Stem cell researcher Shinya Yamanaka, who invented IPS cells in 2006, shared a 2012 Nobel Prize for his discovery.
Although most attention in the media has focused on the potential of IPS cells for directly repairing damaged tissues, scientists found a more immediate use as models for various ailments, including Parkinson's disease and Alzheimer's.
Gage said the stem cell project is focused on getting results that make a difference to patients, not simply piling up research information.
Being able to replicate results is critical; Gage said. Recent studies have found that many research findings of potential therapies don't hold up in clinical testing. This is not only frustrating to patients, but failed clinical trials are expensive, and must be paid for with successful drugs.
"The future of this will require more patients, replication between labs, and standardization of the procedures used," Gage said.
So if the team at Salk has made findings, other labs will be asked to replicate the results. Then the Salk team would re-confirm the finding on additional patients.
Using existing therapies better
UC San Diego Professor of Psychiatry Gregory Light said the stem cell strategy will yield benefits over the long term, but there are current treatments that can help patients right now.
Unfortunately, many treatments aren't being used as effectively as they could be, said Light, who is also director of the Mental Illness, Research, Education and Clinical Center at the VA San Diego Healthcare System. So his work is devoted to using laboratory tests of brain function to predict and monitor response to treatments.
"Right now, treatments are delivered in the absence of information about individual variation in brain function," Light said. "In other words, we use a one-size-fits-all approach to treatment-- there's tremendous variation in who responds and who doesn't."
Assessments of a patient's state of mind rely relies heavily on the patient's own self-reporting of complex inner experiences, which can be flawed because of the condition that needs to be treated, Light said. Assessments by therapists also involves significant subjectivity.
But more objective methods such as noninvasive brain wave monitoring testing can help inform treatment decisions, Light said. The monitoring can establish how a person is likely to respond to a given therapy. This saves time; if the treatment doesn't show signs of working, other treatments can be tried.
It's important to remember that quality treatment involves more than just finding the right medications, Light said. Much work is needed to help patients receive effective cognitive, psychosocial, and vocational interventions to enhance quality of life and outcomes, Light said.
In other words, the spectrum of a patient's life needs needs to be addressed, not just a biochemical imbalance.