“Cancer is one the main causes of death in the US. Our research is focused on understanding how we can harness the power of our immune system to attack and kill cancer cells and cure patients. I chose to join Sanford Burnham Prebys because of their collaborative research culture and state-of-the- art core facilities. I believe that teamwork is the foundation of scientific breakthroughs, and the Institute provides a perfect supportive and friendly environment to achieve this.”
Originally from the Netherlands, Kelly received her BS and MS from Utrecht University, and performed her PhD studies at the Netherlands Cancer Institute in Amsterdam working with Prof. Karin de Visser studying the role of the immune system in the metastatic spread of breast cancer. For her postdoctoral training, Kelly joined the lab of Prof. Max Krummel at the University of California San Francisco to study how tumor-associated myeloid cells affect anti-tumor T cell responses. Kelly is currently setting up her independent research team at Sanford Burnham Prebys.
Education
2016-2023: Postdoctoral Training, University of California San Francisco (Mentor: Prof. Max Krummel, focus on immune evasive cancer)
2017: PhD, Netherlands Cancer Institute Amsterdam/ Leiden University (Mentor: Prof. Karin de Visser, focus on role immune system in breast cancer metastasis, 2011-2016)
2011: MS, Biomedical Sciences, Utrecht University, Netherlands
2008: BS, Biology, Utrecht University, Netherlands
Honors and Recognition
2022: Selected Attendee for SITC Women in Cancer Immunotherapy Network (WIN) Leadership Institute
2022: Selected Attendee for Arthur and Sandra Irving Cancer Immunology Symposium
2022: Ray Owen Poster Award for Outstanding Poster Presentation at 60th Midwinter Conference for Immunologists at Asilomar (sponsored by AAI)
2020-2022: Parker Scholar Award awarded by the Parker Institute for Cancer Immunotherapy (PICI)
2018: Honorable Mention of poster presentation at UCSF/UCB/UCM Immunology Retreat
2018: Poster presentation ‘Excellence in Research Award’ awarded by the National Philanthropic Trust
2017-2019: NWO Rubicon postdoctoral fellowship awarded by the Netherlands Organization for Scientific Research (NWO)
2015: Best presentation award at the annual Tumor Cell Biology meeting of the Dutch Cancer Society (KWF)
2014: Travel scholarship awarded by the Dutch Foundation for Pharmacological Sciences (NSFW)
2010: Master scholarship awarded by the Dutch Cancer Society (KWF)
Memberships
2022-present: Society for Immunotherapy of Cancer (SITC)
2020-present: Parker Institute for Cancer Immunotherapy (PICI)
2012-present: American Association for Cancer Research (AACR)
Related Disease
Breast Cancer, Cancer Biology, Immune Disorders, Inflammation, Innate Immunity, Metastasis, Skin Cancer and Melanoma, Tumor Microenvironment, Tumorigenesis
Phenomena or Processes
Adaptive Immunity, Innate Immunity
Research Models
Mouse, Primary Cells
Techniques and Technologies
Cellular and Molecular Imaging
The Kersten lab studies the interactions between the immune system and cancer.
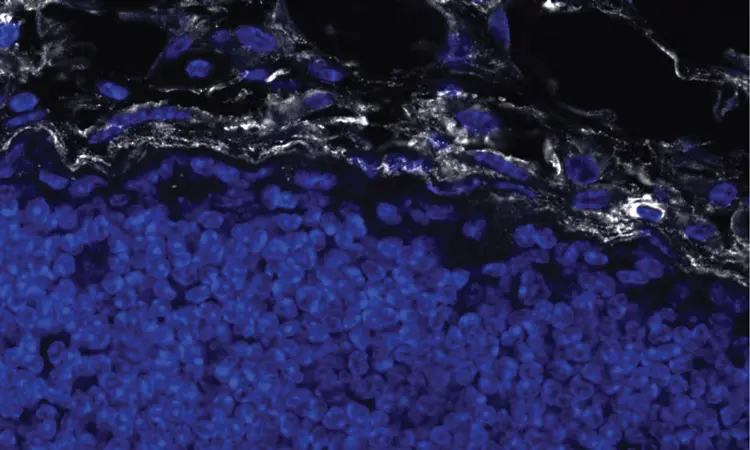
We are fascinated by the crosstalk between the immune system and cancer. Our goal is to understand how cancer cells hijack the normal physiology and function of immune cells to support tumor growth and evade destruction by the immune system.
Kelly Kersten’s Research Report
Cancer immunotherapy, harnessing a patient’s immune system to fight cancer, has revolutionized the way we treat cancer. However, a large proportion of patients do not respond to this type of therapy, and we do not fully understand why. In the Kersten lab, we study how different immune cells affect anti-tumor immunity with the ultimate goal to improve therapies to fight cancer. Research in our lab is focused on understanding how interactions between different immune cells in the tumor microenvironment, specifically macrophages and T cells, affect anti-tumor immunity and responsiveness to immunotherapy. Why do T cells become dysfunctional and exhausted? How do exhausted T cells modulate the composition of immune cells in tumors? And how do macrophages shut down anti-tumor T cells? Our research aims to define the molecular mechanisms that regulate these reciprocal signals to design novel anti-cancer therapies. How immune cells function is highly context-dependent. Upon infiltration in the tumor microenvironment, immune cells face extremely harsh conditions characterized by nutrient deprivation, hypoxia and metabolic challenges resulting in their failure to function properly. We study how different environmental factors impact immune cell phenotype and function, with the goal to optimize their cancer-killing properties.
 Dec 12, 2025
Dec 12, 2025Sanford Burnham Prebys scientists garner eight cancer research grants from Curebound to advance therapeutic treatments and cures
Dec 12, 2025Ten scientists at Sanford Burnham Prebys Medical Discovery Institute were awarded eight grants yesterday from Curebound, a San Diego-based philanthropic organization
 Sep 2, 2025
Sep 2, 2025How Cellular Crosstalk Translates into Idiopathic Pulmonary Fibrosis
Sep 2, 2025Rare but deadly condition begins with metabolic changes to make a pro-fibrotic metabolite.
 May 2, 2025
May 2, 2025Kelly Kersten awarded Melanoma Research Alliance grant to support research on melanoma immunotherapy
May 2, 2025The newly created award is part of the alliance’s $9.3 million commitment to melanoma research funding in 2025.
 Oct 31, 2024
Oct 31, 2024Raising awareness of breast cancer research at Sanford Burnham Prebys
Oct 31, 2024The October Science Connect Series event was themed around Breast Cancer Awareness Month.
 Jun 4, 2024
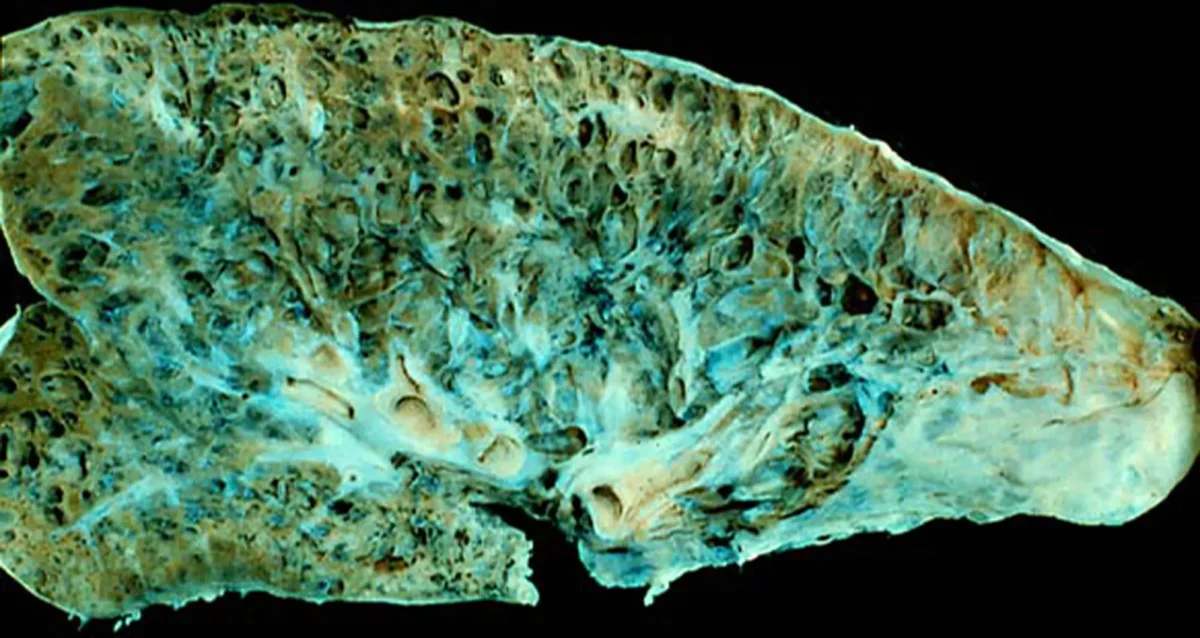
Jun 4, 2024How tumor stiffness alters immune cell behavior to escape destruction
Jun 4, 2024Immunotherapy is based on harnessing a person’s own immune system to attack cancer cells. However, patients with certain tumors do…
 Feb 7, 2024
Feb 7, 2024Speaking of International Day of Women and Girls in Science
Feb 7, 2024Designated by the United Nations, the 9th International Day of Women and Girls in Science is Sunday, February 11, preceded…
