Scientists at the Sanford Burnham Prebys Medical Discovery Institute (SBP) have identified over 100 new genetic regions that affect the immune response to cancer. The findings, published in Cancer Immunology Research, could inform the development of future immunotherapies—treatments that enhance the immune system’s ability to kill tumors.
“By analyzing a large public genomic database, we found 122 potential immune response drivers—genetic regions in which mutations correlate with the presence or absence of immune cells infiltrating the tumors,” said lead author Eduard Porta-Pardo, PhD, a postdoctoral fellow at SBP. “While several of these correspond to proteins with known roles in immune response, many others offer new directions for cancer immunology research, which could point to new targets for immunotherapy.”
Immunotherapy has been heralded as a turning point in cancer because it can treat even advanced cases that have spread to other organs. Several drugs in this class are now widely used and often lead to remarkable success, eradicating or dramatically shrinking tumors and preventing recurrence.
Most current immunotherapies rely on a similar strategy—releasing the brakes on the immune system. These treatments are powerful if the tumor is recognized by the immune system as a threat and allows immune cell infiltration, but some cancers remain undercover or block immune cell entry into the tumor in as yet unknown ways.
“To develop immunotherapies that are relevant to a wide range of cancers, we need to know a lot more about how the immune system interacts with tumors,” said Adam Godzik, PhD, professor and director of the Bioinformatics and Structural Biology Program and senior author of the study. “Our study provides many new leads for this endeavor.”
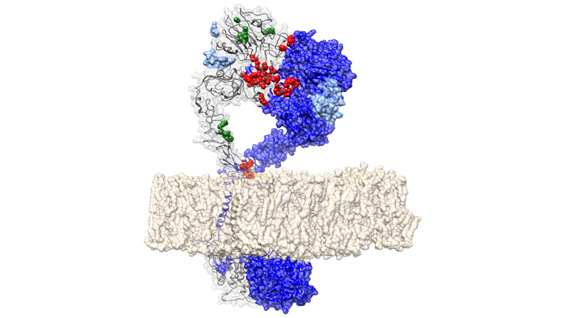
“We are exploring cancer mutations at fine resolution by accounting for the fact that mutations can affect the encoded protein in different ways depending on where the resulting change is located,” commented Porta-Pardo. “Our algorithm, domainXplorer, identifies correlations between a phenotype, in this case the amount of immune cells in the tumor, and mutations in individual protein domains—parts of a protein with distinct functions.
“This work emphasizes the value of open data,” Godzik added. “Because we could access genomic data from over 5,000 tumor samples from The Cancer Genome Atlas (TCGA), we could jump straight to analysis without having to set up a big collaborative network to gather and sequence so many samples.”
“Our plan for the next phase of this research is to use this algorithm to search for genetic regions correlating with the levels of specific immune cell types within the tumor, which will reveal further details of cancer immunology.”