New research on four variants in the EPHA1 gene reveals how its genetic typos may contribute to risk of dementia
Upon inspecting the DNA sequences in patients suffering from Alzheimer’s disease, scientists have found evidence of an inconspicuous conspirator.
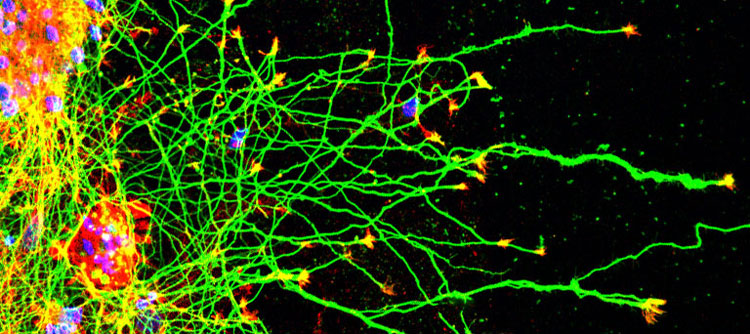
The EPHA1 gene contains the blueprint for the EPHA1 receptor protein, one of 14 such receptor proteins in the Eph receptor family. Relatively little is known about EPHA1 when compared to many of its siblings, making it difficult for researchers to ascertain why changes in its source code would contribute to such a debilitating disease.
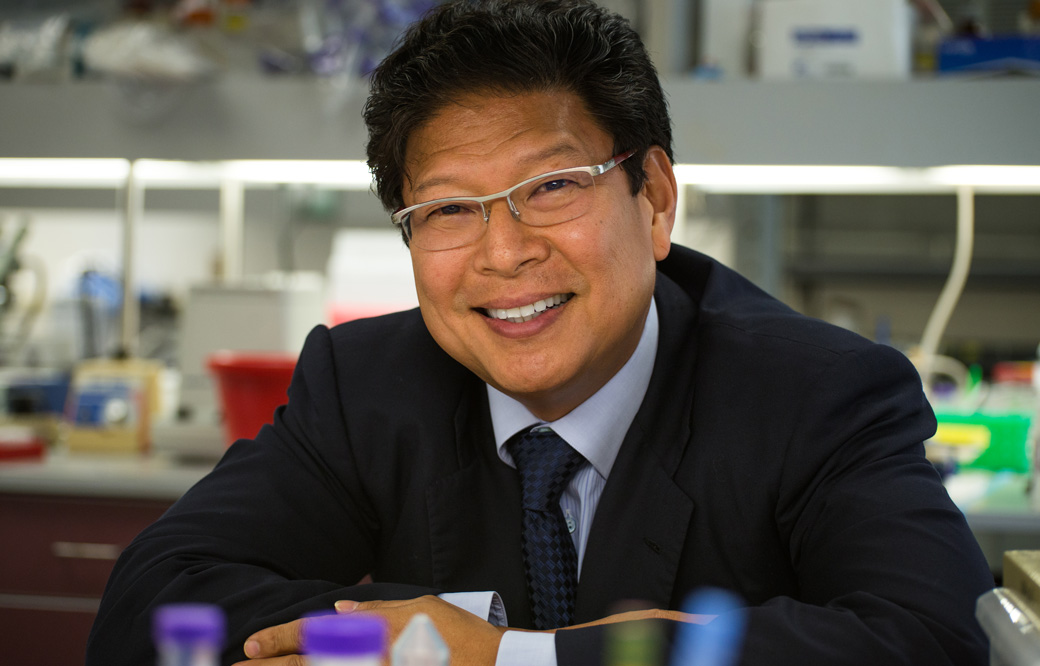
Scientists at Sanford Burnham Prebys published results on December 18, 2024, in the Journal of Biological Chemistry, detailing the effects of four miniature mutations of just a single typo each in the sequence of nucleotides forming the EPHA1 gene.
These seemingly minor mutations are known as single nucleotide polymorphisms (SNPs), and they can lead to larger issues depending on where the typos fall in the sequence of a gene. The Sanford Burnham Prebys team focused on four missense mutations that are caused when SNPs result in different amino acids being used to build the EPHA1 receptor protein.
“Our data show that all four Alzheimer’s mutations we have characterized disrupt EPHA1 physiological signaling, and that the specific effects depend on the particular mutation,” said Elena Pasquale, PhD, professor in the Cancer Metabolism and Microenvironment Program at Sanford Burnham Prebys.
The team reported that the functional consequences of EPHA1 missense mutations identified in patients suffering from Alzheimer’s disease included misplacement of EPHA1 within cells, decreased protein stability and dysregulated signaling.
“To continue advancing knowledge on this topic, more work is needed to uncover the physiological role of the different EPHA1 signaling features and how their disruption may lead to neurodegeneration,” said Pasquale.
Additional authors on the study from Sanford Burnham Prebys include Mike Matsumoto and Sara Lombardi, PhD. Maricel Gomez-Soler, PhD, now works at Crinetics Pharmaceuticals in San Diego. Bernhard C. Lechtenberg, PhD, now works at the Walter and Eliza Hall Institute of Medical Research in Parkville, Australia.