Hope’s research aims to help cancer immunotherapy work for more people
It’s not an overstatement to say that immunotherapy—an approach that uses our own immune system to kill a tumor—has revolutionized the treatment of cancer. Doctors continue to report incredible results, including tough-to-treat tumors seemingly melting away. However, the treatment doesn’t work for everyone, and even if it does work initially, it often stops working as time goes on.
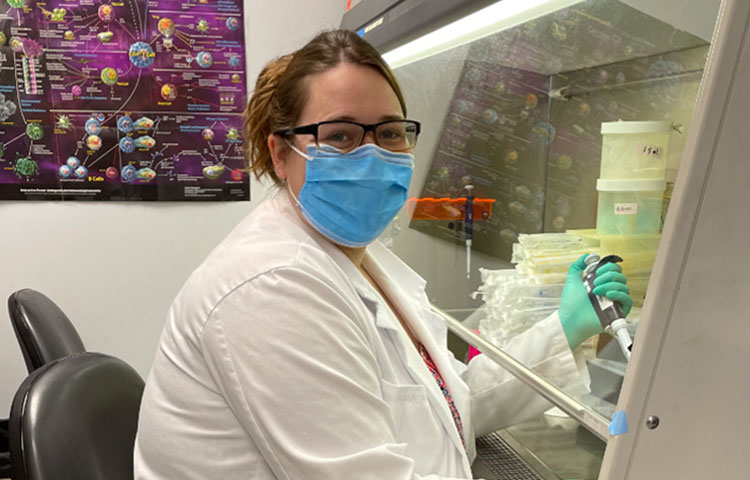
Jennifer Hope, PhD, a postdoctoral researcher in the Bradley lab at Sanford Burnham Prebys, is working to find ways to make cancer immunotherapy work for more people. We caught up with her as she prepared to take the virtual stage at the Diversity and Science Lecture Series at UC San Diego (DASL) to learn more about what she wishes people knew about science and whom she admires.
Did you always know you wanted to be a scientist?
I always had an interest in science, but at first I wanted to go a totally different route. I was an athlete in high school and college—I played tennis—and really wanted to go into sports medicine. Then I had my first real experience being in a lab in college, and I was hooked. I liked how hands-on it was and how I could keep asking questions. As my family knows, I’ve always been one to ask a lot of questions and always ask why. I found that being in the lab that was my opportunity to keep coming up with new questions, and finding answers that will impact people’s lives.
What do you research, and what is your greatest hope for your work?
I’m trying to understand why the immune system—specifically, T cells—seems to turn a “blind eye” to tumors, which it doesn’t do to other foreign invaders like viruses. My ultimate hope is that we use this information to create better cancer immunotherapies, particularly for skin cancer, which is still really deadly.
What do you wish people knew about science?
That it can be a lot of fun! Most people have this perception of science as being very boring. You see X and you do Y. That part can be true. But there’s a lot of opportunity for creativity and to come up with different ways to ask the same question. Some of the best scientists are incredibly creative people.
How would your coworkers describe you?
Motivated and always willing to try new things.
When you aren’t working, where can you be found?
Reading a book. My family started a book club to stay connected during the pandemic. We just read The Food Explorer by Daniel Evan Stone, which was fascinating. It’s about a botanist who is responsible for transforming what food looked like in the U.S. at the turn of the century. I don’t want to give too much away, but it’s because of him that we have cherry blossoms in Washington D.C., and regulations on importing seeds.
Whom do you admire, and why?
My parents. It sounds cliché, but it’s true. They have always been the biggest supporters of my dreams, whether career or personal.
One example that pops into my head is when I was getting my PhD, and my PI moved from Philadelphia to the Netherlands. I had the opportunity to move, too, if I wished. This was obviously a huge step, and I called my parents to talk it through. Immediately, the conversation was about how this would benefit me—the risks and the advantages—and they said they would support me if I wanted to go or not. That meant, and means, the world to me. Ultimately, I did go, and it was an incredible opportunity that I don’t regret at all.
What do you wish people knew about Sanford Burnham Prebys?
That everyone is willing to help each other. You don’t see that everywhere. It is proof that you can do science at an exceptional level without competing with each other.