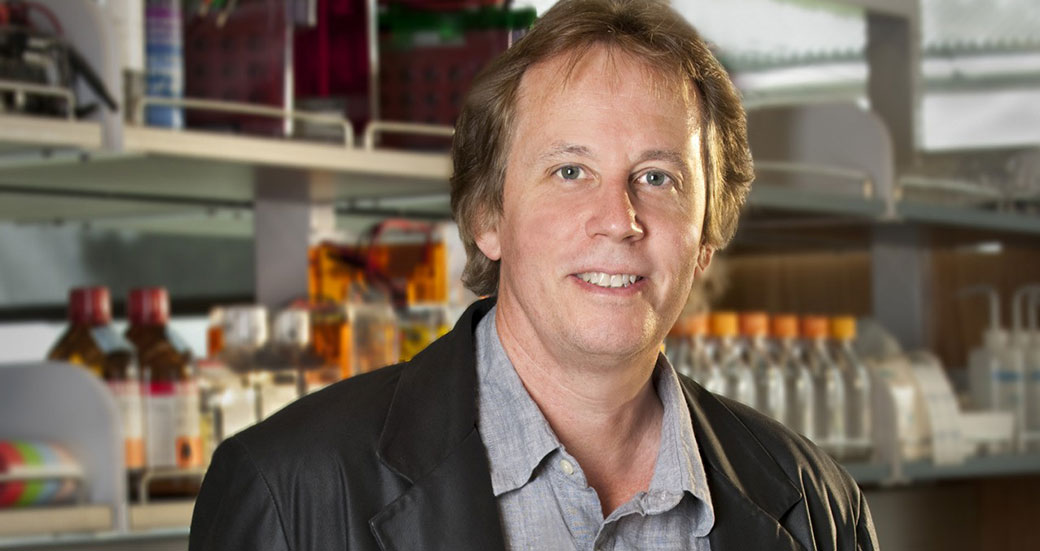
A multidisciplinary team of scientists led by Jamey Marth, PhD, professor in the NCI-designated Cancer Center and director of UC Santa Barbara’s Center for Nanomedicine, is poised to undertake a major biomedical research initiative focused on the escalating problem of sepsis, the body’s abnormal response to severe infections.
The multi-investigator program will be supported by a five-year, $12.8 million research grant from the National Institutes of Health (NIH).
“Millions of people are diagnosed with sepsis each year worldwide, and on average 30 percent die from the complications of sepsis. No new effective treatments have been developed in decades,” said Marth.
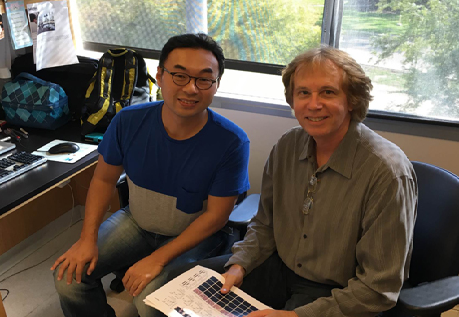
Playing a lead role in the translational component is Jeffrey Fried, MD, an acute care physician at Santa Barbara Cottage Hospital and an expert in sepsis. Fried and Marth have collaborated over the past four years.
“With Dr. Fried’s expertise, we have already made unexpected discoveries pertaining to human sepsis,” Marth said.
“While we have made great strides at our hospital in reducing the mortality of sepsis by two-thirds over the past 11 years, we have reached a plateau of what we can accomplish without new treatments,” Fried explained. “Marth and his co-investigators have done seminal work in investigating the molecular basis of sepsis. This work should translate into the development of radically different and more effective approaches to treating sepsis in the future.”
Additional contributing biomedical scientists and clinicians include UC San Diego faculty member Jeffrey Esko, PhD, an expert in the mechanisms of blood-based diseases, and Dzung Le, MD, PhD, head of the clinical hematology and coagulation laboratory at UC San Diego’s Hillcrest and Thornton hospitals. Jeffrey Smith, PhD, also a professor in SBP’s NCI-designated Cancer Center, brings leading expertise in mass spectrometry methods applied to blood systems.
“I look forward to contributing to this potentially transformative research,” said Smith. “The proteomics analyses at SBP will link regulation of specific blood proteins to disease states, which should point to targets for future therapeutic development.”
The program will also benefit from the involvement of renowned scientists and clinicians on its advisory board. “Sepsis remains the leading killer of patients in intensive care units and there are no approved medications,” said advisory board member Victor Nizet, MD, PhD, chief of the Division of Host-Microbe Systems and Therapeutics at UC San Diego’s School of Medicine. “The highly innovative discoveries by Jamey Marth and his team have inspired a rethinking of how blood components respond to severe infection and suggest new ways to restore normal function and protect vital organs from injury.”
Marth noted the program’s potential to reduce the frequency of disability and death in patients diagnosed with sepsis. “We have an extraordinary opportunity to achieve major advances in the understanding and treatment of sepsis,” he said.
This post is based on a press release from UC Santa Barbara.
Venn diagram portraying relationships among causes and risk factors for sepsis. “SIRS” refers to systemic inflammatory response syndrome. Diagram provided by Jamey Marth.