The National Institutes of Health recognizes April as National Stress Awareness Month, with the goal of bringing awareness to the health impact of stress.
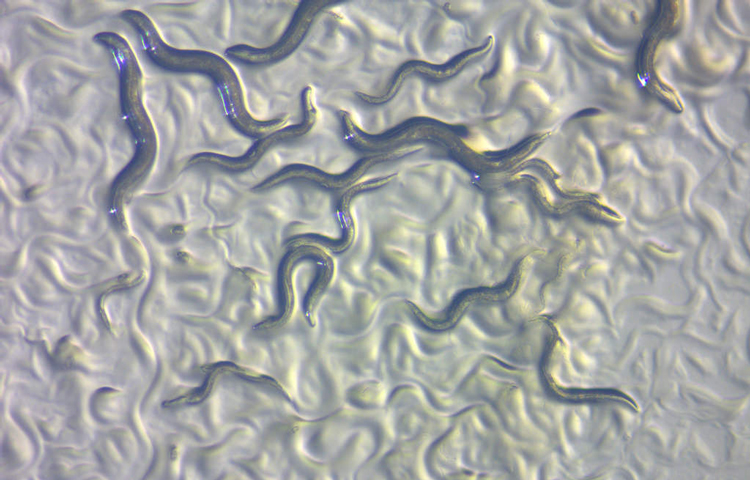
Stress comes in many forms—from the psychological stress we experience during difficult moments to the biological stress in our smallest cells. At Sanford Burnham Prebys, Assistant Professor Caroline Kumsta, PhD, uses small worms (nematodes) to study the negative relationship between cellular stress and aging (yes, aging can be stressful!). On the flip side, she’s also exploring how we can use small amounts of stress to improve health and potentially treat neurodegenerative diseases.
We spoke to Kumsta about her research to learn more about how nematodes, stress and neurodegenerative diseases are all related.
Why do you work with nematodes?
Nematodes are very good for aging research because they have a short life span—only a few weeks—so we can measure the effects of aging within a reasonable amount of time. Another reason why we like these worms is because we can measure stress responses in more than individual cells. We can use nematodes to study broader, more systemic responses, as well as how stress responses are communicated from tissue to tissue. We can only see these effects if we look at how stress responses are orchestrated across the entire organism. Even though worms don’t look like us, a lot of the basic biological machinery we study is the same as in humans because stress responses evolved a long, long time ago.
How do worms help you study aging and cellular stress responses?
“What doesn’t kill you makes you stronger” is true in biology—in other words, small amounts of stress can actually be beneficial for organisms, including humans. We’re studying this idea in nematodes by giving them a small heat shock early in their lives, almost like giving them a few minutes in a sauna. The heat triggers stress responses in the worms at the cellular level, and one of these responses is that the worms’ cells induce a cellular recycling process, called autophagy. Autophagy recycles cellular components and helps keep cells healthy and free from debris. This is a beneficial process that helps increase the life span of the worms. My team is exploring how this process works and figuring out how we can use it to fight diseases.
How can your work in nematodes help us study human diseases?
Our main target is neurodegenerative diseases. One of the drivers of diseases like Alzheimer’s, Parkinson’s or Huntington’s disease is that proteins accumulate in the brain in aggregates or clumps. We’ve seen that nematodes that have had a heat shock early in their lives have reduced clumping of disease-relevant proteins. This is because when autophagy kicks in as a stress response, it helps slow the accumulation of these clumpy proteins. We’re ultimately looking for ways to boost the cellular recycling process in humans as a way to treat degenerative diseases. We can imagine heat therapy as a treatment intervention, and we are currently developing methods of measuring autophagy status in humans so that we will be able to test potential interventions.