Neurodegenerative diseases are a major worldwide health problem, and researchers are hunting new strategies to combat them. One approach is to find the mutations that cause these diseases and design therapies to counteract them. But scientists can also pursue another strategy—identify molecules that protect neurons from harm.
SBP’s Laszlo Nagy, MD, PhD, may have found one of these. Nagy is working on gene regulation and epigenomics—so neurons are not his primary beat. But in a recent study published in The Journal of Neuroscience, he and colleagues have shown that the enzyme PRMT8 can protect aging motor neurons from stress, which could have therapeutic implications.
“We stumbled on this molecule PRMT8, which is a protein methyltransferase (an enzyme that adds methyl molecules to control protein expression and activity) while studying stem cell differentiation,” says Nagy. “When the molecule is not there, the motor neurons are less stress resistant. They are vulnerable to changes in their inner circuitry, including DNA damage, and they eventually die.”
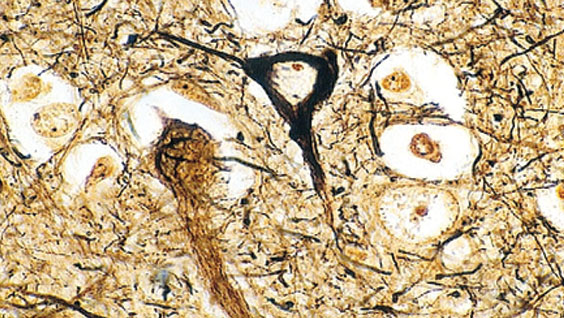
Stress management is particularly important in motor neurons, which connect the central nervous system to muscles. Mature motor neurons cannot divide anymore and must live a long time. Once they die, they are lost forever.
In the study, the lab found that motor neurons in animals without PRMT8 developed a number of issues. The cells had DNA breaks and other problems that slowly killed them off. As motor neurons died, the animals gradually lost muscle strength.
“In older animals, they were having difficulty coordinating their movements,” says Nagy.
Because PRMT8 has the potential to protect motor neurons, it could be a compelling drug target. Boosting the enzyme could help slow a number of neurodegenerative conditions, including ALS. In addition, because the enzyme is only found in the central nervous system, it offers a selective target. This is particularly important, since adding stress protection to dividing cells could cause cancer.
Now that they have identified PRMT8’s neuroprotective benefits, Nagy and colleagues are taking the next step—looking for agents that could make the enzyme more active and potentially help motor neurons resist disease and live longer.
“We’re trying to identify a small molecule that would enhance PRMT8, so we could specifically modulate its activity,” he says.