Over the past three decades, researchers have been investigating an important cell communication system called the “Eph system,” and the evidence implicating the system in cancer is staggering.
The Eph system is comprised of multiple Eph receptors and their ligands—ephrins—and are involved in contact-dependent communication between cells. They play essential roles in regulating various cellular processes.
Modern studies have shed light on the Eph system’s role in tumor expansion, invasiveness, metastasis, cancer stem cell maintenance and therapy resistance.
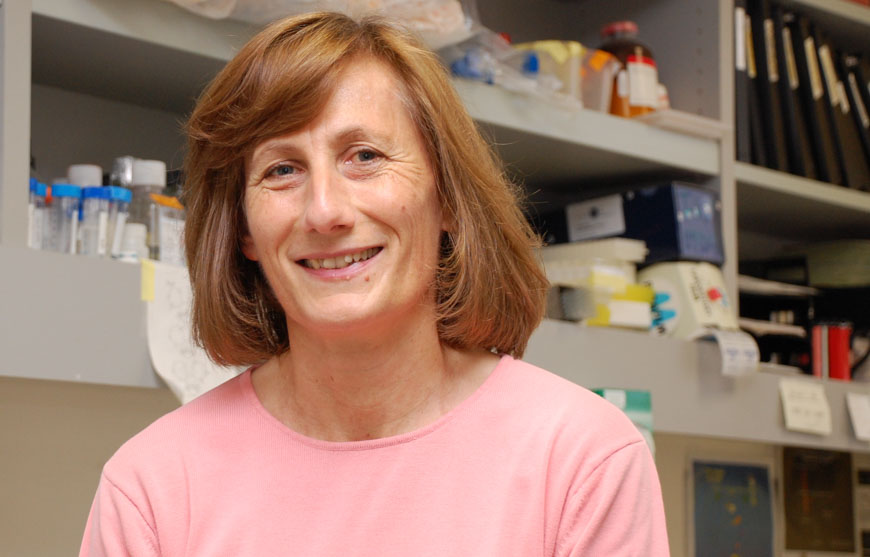
This month, Elena Pasquale, PhD, published a review in Nature Reviews Cancer that summarizes the current state of research on the Eph system and its links to cancer progression and drug resistance.
“The Eph system has many critical functions during the development of tissues and organs, but it also has the capacity to either promote or suppress cancer progression and malignancy” says Pasquale. “In cancer, the activities of the Eph system can differ depending on the circumstances—for example, which Eph receptors and ligands are present in a tumor cell, the types of tumor cells in which they function, and the characteristics of these cells.”
“It’s this remarkable versatility that makes the Eph system a compelling but also challenging target for potential therapies,” says Pasquale.
“The aims of this review were to comprehensively survey the large body of data regarding various aspects related to Eph signaling in tumors and to highlight potential strategies for therapeutic targeting,” says Pasquale. “Overall, while significant progress has been made in deciphering the Eph system in cancer, there is much more to learn.
“Gaining a deeper understanding of how the Eph system functions in cancer is challenging but will be essential for the development of targeted therapies and personalized treatment approaches for patients.”