Almost 6 million people in the US have failing hearts, which can arise following heart attacks, longstanding high blood pressure, defective heart valves or genetic disorders, among other causes. While management of heart failure (HF) is improving, only 50% of patients will survive five years after diagnosis. No current treatments directly treat the disease, particularly at early stages, so development of new preventive or therapeutic drugs could make an enormous difference for patients.
A new study from the laboratory of Daniel Kelly, MD, Tavistock Distinguished Professor and Scientific Director of SBP’s Lake Nona campus, published in JCI Insight, shows that muscle cells in failing hearts contain high levels of metabolites that modify enzymes in mitochondria, the cell’s energy power plant. The enzyme modifications reduce the ability of mitochondria to make enough ATP to power the heart. Targeting this newly identified pathway may lead to drugs that slow the progression of HF.
HF is known to result, in part, from insufficient supplies of ATP—the energy currency within cells—in heart muscle. But the factors that slow ATP production in a failing heart remain unclear. Kelly’s recent study sheds light on this issue, identifying a pathological cycle that contributes to HF.
“Our findings point to a detrimental cycle that progressively decreases ATP production in heart muscle cells. When the heart’s energy demand increases during the early stages of heart failure due, for example, to a heart attack, a particular metabolite called acetyl-CoA begins to accumulate. This metabolite modifies mitochondrial enzymes, reducing their efficiency, which further increases accumulation of the metabolite,” explains Kelly. “This vicious cycle goes on and on until eventually the heart becomes starved of energy and cannot support pump function.”
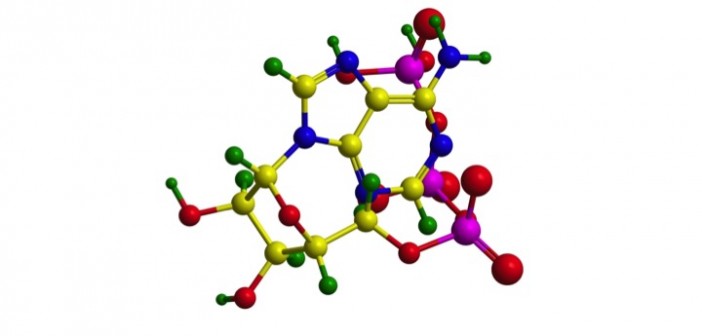
Here are the details: The Kelly research team, part of the Center for Metabolic Origins of Disease, followed up on earlier observations that levels of acetyl-CoA are increased in failing hearts in mice. Since high levels of acetyl-CoA can drive protein acetylation, they looked for acetylated proteins in mitochondria, and found that many mitochondrial enzymes were indeed hyperacetylated. They went on to demonstrate that this also occurs in the failing human heart.
In a further analysis, succinate dehydrogenase A, one of the key enzymes needed to generate ATP, was genetically modified to mirror an acetylated version. When tested, the ‘mock’ acetylated protein was less able to perform its ATP-generating responsibilities. The findings support the fact that the enzymes needed to support ATP generation are hindered if acetylated.
Next steps: These results raise several questions, including how metabolic changes drive the accumulation of acetyl-CoA and how excess acetyl-CoA leads to protein acetylation.
“In the next phase of this research, we plan to identify specific players driving protein acetylation that could be targeted by future drugs,” adds Kelly.
The paper is available online here.