Understanding the crucial ingredient in bile may unlock the potential of treatments that help patients’ immune systems eliminate cancer
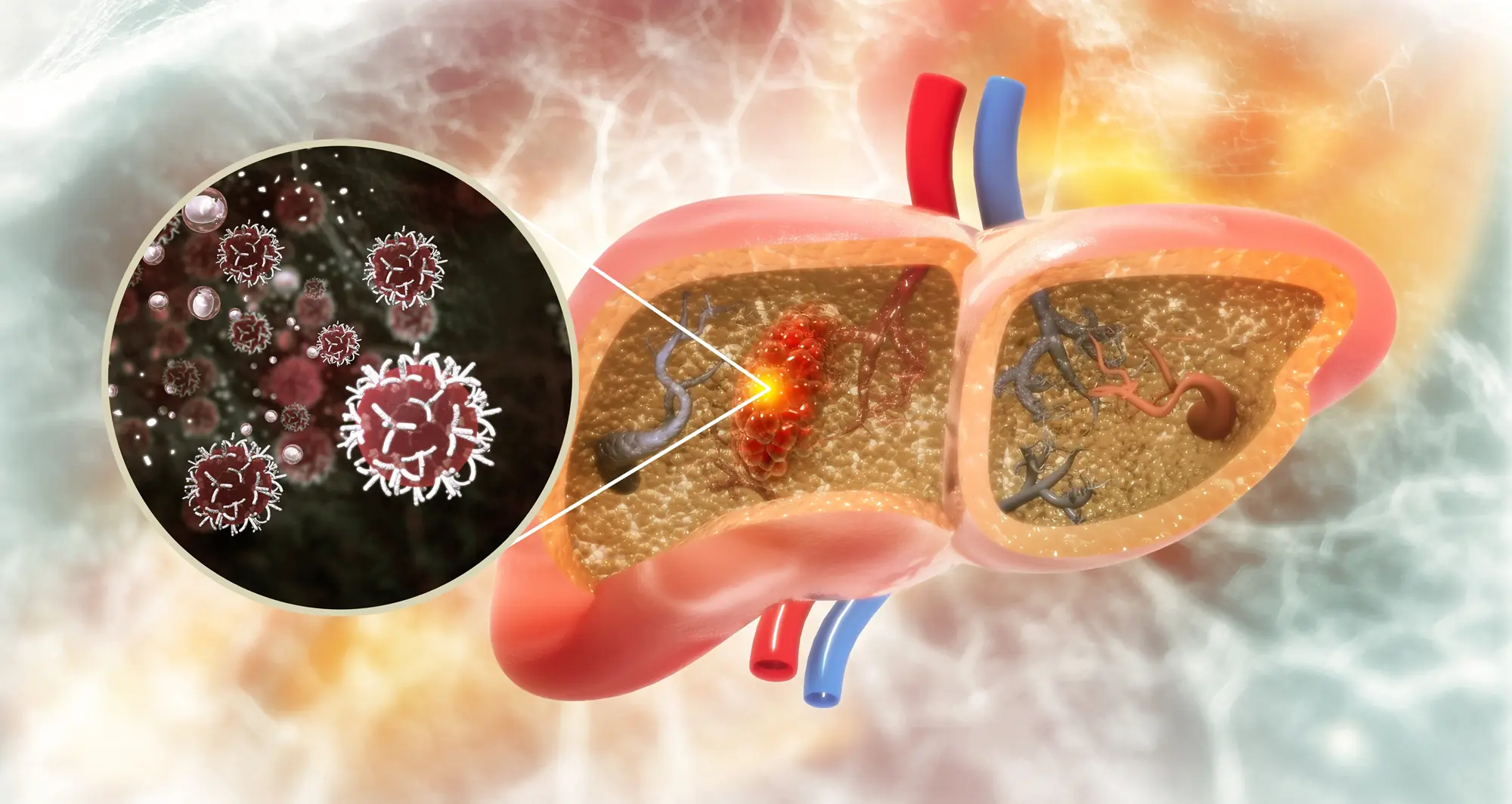
Hepatocellular carcinoma (HCC) is the most common liver cancer and a growing threat to public health across the globe due to the rising rate of fatty liver disease.
Liver cancer is difficult to treat as it often causes few if any symptoms early on, so it tends to be diagnosed at later, more aggressive stages. While immunotherapies that supercharge patients’ immune systems have proven effective in some cancers, this approach has had limited success in patients suffering from HCC or other forms of the disease.
Scientists are investigating the unique qualities of different tissues that may explain why the effectiveness of immunotherapy varies depending on the location of a tumor. The liver is known to have a flexible immune system capable of defending itself when necessary while not overreacting to a constant flood of foreign materials from digesting food, including metabolic byproducts from bacteria residing in the gut microbiome.
Transplant surgeons see the unique properties of the liver’s immune system firsthand when transplanted livers are typically integrated by recipients with only a low dose of immunosuppressive drugs. This ability to maintain immune tolerance, however, may reduce the ability of the liver’s immune system to find and destroy cancer cells, even when that capability is enhanced by immunotherapy.
In a paper published January 9, 2025, in Science, scientists at Sanford Burnham Prebys, the Salk Institute, the University of California San Diego, Columbia University Irving Medical Center, Memorial Sloan Kettering Cancer Center and the Geisel School of Medicine at Dartmouth, found that a critical ingredient in bile hinders the liver’s immune response against cancer.
Bile is a fluid made by the liver that assists in breaking down fats during digestion. This function is made possible by steroidal acids known as bile acids. The scientists found an increased amount of bile acids in tumor samples from patients with HCC. The team also found that genes involved in creating bile acids were being transcribed to make proteins and enzymes at an abnormally high rate in human samples and in mice genetically modified to develop liver cancer.
The authors went on to remove genes related to bile acid construction to demonstrate that mice without these blueprints developed fewer, smaller tumors. In addition, the liver’s T cells — the primary anti-tumor immune cells — were able to dig deeper into tumors and persist for longer without the immunosuppressive effects of certain bile acids.
“These findings underscore a new appreciation for the influence of bile acids on the liver’s immune system,” said Debanjan Dhar, PhD, associate professor in the Cancer Genome and Epigenetics Program at Sanford Burnham Prebys and coauthor on the study. More research is needed to test the potential use of drugs to directly inhibit certain bile acids or bile acid receptors as a therapeutic strategy to reduce liver cancer growth.

Debanjan Dhar, PhD, is an associate professor in the Cancer Genome and Epigenetics Program at Sanford Burnham Prebys.

Peter Adams, PhD, is the director of the Cancer Genome and Epigenetics Program at Sanford Burnham Prebys.
It may also be possible to achieve this effect through dietary changes that alter the microbiome and result in modified bile acid production. Based on their findings, the research team suggests that this could be done by using ursodeoxycholic acid, a bile acid that currently is used to treat an autoimmune condition called primary biliary cholangitis. The acid is found at high levels in bear bile, which has served for thousands of years as a treatment in traditional Chinese medicine.
“Given the safety profile of ursodeoxycholic acid and the limited effectiveness of immunotherapy on liver cancer, this study shows significant potential for testing this bile acid as a combination treatment for patients with HCC,” said Peter Adams, PhD, director of the Cancer Genome and Epigenetics Program at Sanford Burnham Prebys and coauthor on the study.
Susan Kaech, PhD, NOMIS Chair, professor and director of the NOMIS Center for Immunobiology and Microbial Pathogenesis at the Salk Institute is the senior and corresponding author on the study.
Siva Karthik Varanasi, PhD, assistant professor at the UMass Chan Medical School and a former postdoctoral fellow in the Kaech lab at the Salk Institute, is first author on the manuscript.
Additional authors include:
- Souradipta Ganguly, Marcos G. Teneche and Aaron Havas, from Sanford Burnham Prebys
- Dan Chen, Melissa A. Johnson, Kathryn Lande, Michael A. LaPorta, Filipe Araujo Hoffmann, Thomas H. Mann, Eduardo Casillas, Kailash C. Mangalhara, Varsha Mathew, Ming Sun, Yagmur Farsakoglu, Timothy Chen, Bianca Parisi, Shaunak Deota, H. Kay Chung, Satchidananda Panda, April E. Williams and Gerald S. Shadel, from the Salk Institute
- Yingluo Liu, Cayla M. Miller, Jin Lee and Gen-Sheng Feng, from the University of California San Diego
- Isaac J. Jensen and Donna L. Farber, from Columbia University Irving Medical Center
- Andrea Schietinger from Memorial Sloan Kettering Cancer Center
- Mark S. Sundrud from the Geisel School of Medicine at Dartmouth
Wolfram Goessling, MD, PhD, the Robert H. Ebert Associate Professor of Medicine and associate professor of Health Sciences and Technology at Harvard Medical School, authored a Perspective article on the new study in Science called, “Ena-bile-ing liver cancer growth.”