Renowned data scientist Paul Boutros, PhD, MBA, has been named the new director of the National Cancer Institute-designated cancer center at Sanford Burnham Prebys Medical Discovery Institute.
He is the first computational biologist to oversee an NCI-designated cancer center, a network of 73 basic, clinical and comprehensive centers created as part of the National Cancer Act of 1971.
The cancer center at Sanford Burnham Prebys was established in 1981, and is one of only seven basic laboratory cancer centers in the nation.
Boutros will also hold the titles of senior vice president, data sciences and professor.
Boutros comes to Sanford Burnham Prebys from UCLA, where he was a professor in the departments of human genetics and urology at the David Geffen School of Medicine at UCLA and interim vice dean for research.
He is celebrated for his work in using artificial intelligence, machine learning and the untapped potential of computational science to analyze the massive data sets generated by modern cancer research and vital to designing original and forward-looking studies.
Boutros’ lab and collaborators focus on how the diverse elements of clinical, molecular and imaging data can be linked and leveraged to personalize therapies for cancer patients. Specifically, Boutros seeks to identify biomarkers that can help ensure cancer therapies are selected for maximum benefit and minimum harm.
“Paul is a pioneer,” said David A. Brenner, MD, president and CEO of Sanford Burnham Prebys. “His work is both expansive and probing. He’s showing how today’s rapidly evolving computational tools can answer questions that were once deemed overwhelming, if not impossible.
“It’s his over-the-horizon thinking that is so exciting. Cancer research is transforming. Data science is becoming increasingly elemental to expanding and advancing progress in addressing the more than 200 types of cancer that literally affect tens of millions of Americans and many, many more around the world.
“Paul will help accelerate those achievements, and further elevate the reputation of the cancer center at Sanford Burnham Prebys, combined with partners like the Center for Therapeutic Discoveries, as leaders in the field.”
Boutros earned his BSc degree from the University of Waterloo in Chemistry in 2004 and his PhD degree from the University of Toronto in medical biophysics in 2008. At Toronto, he also earned an executive MBA from the Rotman School of Management.
In 2008, Boutros began his research career at the Ontario Institute for Cancer Research in Canada, first as a fellow (2008–2010) and then as a principal investigator (2010–2018). He moved to UCLA in 2018.
He has published more than 200 peer-reviewed papers and received numerous honors, including the Prostate Cancer Canada Rising Star in Prostate Cancer Research award, the Terry Fox New Investigator Award, the University of Waterloo Young Alumni Award and the Early Career Graduate Student Teaching Award. In 2018 he was awarded the Dorval Prize by the Canadian Cancer Society, recognizing the best national early career investigator.
About the NCI-designated Cancer Center at Sanford Burnham Prebys
Established in 1981, the cancer center at Sanford Burnham Prebys Medical Discovery Institute is one of only seven National Cancer Institute-designated basic laboratories in the nation. Its mission is to answer fundamental questions in cancer biology and to use that new knowledge to address unmet clinical needs by conducting original translational studies.
Faculty expertise spans many specialties, from cell biology and immunology to epigenetics, metabolism, aging and computational science. Capabilities are further enhanced by close collaboration with the Center for Therapeutics Discovery and the Center for Data Science and Artificial Intelligence, both also at Sanford Burnham Prebys.
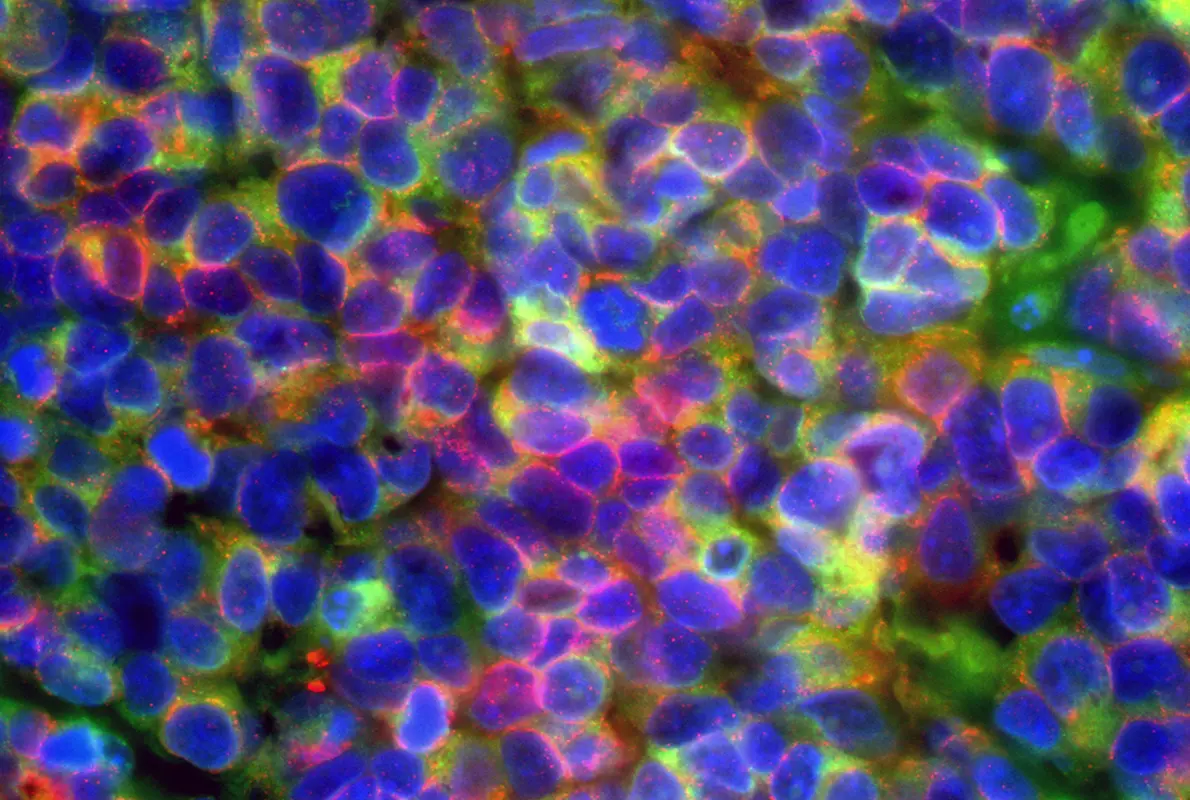
Microscopic image of small cell neuroendocrine prostate cancer, with cancer cells expressing diagnostic prostate cancer markers in green and red. Blue areas indicate cell nuclei. Image courtesy of Jung Wook Park and Owen Witte, UCLA.
Exercise and Prostate Cancer
Prostate cancer is the second-leading cause of death in American men, after lung cancer. Approximately 1 in 44 men will die of the disease, according to the American Cancer Society (ACS); nearly 36,000 men in 2025 alone.
For low-risk, slow-growing prostate cancers, the first course of treatment is often active surveillance, but more aggressive treatments include surgery, radiation and hormonal, chemo and immunotherapies.
In 2024, senior author Paul Boutros, PhD, and colleagues published a paper in JAMA Oncology describing a Phase I, decentralized and nonrandomized controlled trial to investigate whether exercise therapy for men with diagnosed prostate cancer might improve their prognoses and reduce the risk of prostate cancer death.
Specifically, the scientists would look at whether exercise improved two key biomarkers associated with better outcomes.
“It was already suspected that exercise beneficially impacted prostate cancer progression and spread, but the collected data was typically self-reported, observational and not really actionable,” said Boutros. “We wanted to know how much exercise under known and controlled conditions affected patients’ conditions, not unlike how drugs are tested and prescribed.”
Leveraging multiple technologies and computational tools in the trial, 53 inactive men with prostate cancer, ages 47 to 74 and living across the country, were provided at home with a treadmill, iPad, smartwatch, continual glucose monitor, blood pressure cuff and digital scale and assigned different levels of moderate-intensity treadmill walking, from 90 to 450 minutes per week. All of their activities would be conducted remotely with real-time monitoring and oversight by exercise physiologists.
The men were then measured for two biomarkers: Ki-67, a protein that indicates how fast cancer cells are dividing and proliferating, and prostate specific antigen (PSA), a well-established marker for prostate cancer risk and progression.
The researchers arrived at two important conclusions. First, previously inactive men were consistently able to complete high levels of exercise therapy with no adverse effects. Second, the scientists determined that 225 minutes (3 hours, 45 minutes) per week was the optimal amount of exercise to reduce the risk of prostate cancer harm. Fewer minutes did not impact the biomarkers; more minutes changed the biomarkers only slightly.
Boutros and colleagues have since launched a multi-institution phase 2 clinical trial to better understand how the targeted exercise amount impacts the progression of prostate cancer compared to participants following their usual exercise routines.
