Study shows how new chemical probes can count individual enzymes and discern their activity levels, may inform discovery of new treatments
Cells operate on rules not vibes, including when on the precipice of persisting or perishing. Yet, with prior research methods, scientists studying this phenomenon had to infer how cells choose to sustain themselves or self-destruct based on the output of their protein factories.
While much more advanced than a pundit’s vibe check, these analyses were constrained by the inability to account for the activity of these proteins after their construction.
Scientists at Sanford Burnham Prebys Medical Discovery Institute and Wroclaw University of Science and Technology published findings January 10, 2026, in Cell Reports demonstrating a new approach for measuring their activity. The researchers also revealed a more complicated picture in which protein activation cannot always be presumed by protein production.
Many cells in our bodies are routinely monitored for signs that they need to be removed. Like a gardener pruning dead or diseased branches, cells that are dysfunctional due to aging or mutation are removed through a process of programmed cell death, known as apoptosis. One of cancer’s calling cards is that cancerous cells ignore apoptosis and grow to become harmful tumors.
“Scientists have defined a lot of the cellular signals involved in apoptosis,” said Guy Salvesen, PhD, professor emeritus at Sanford Burnham Prebys and senior and co-corresponding author of the manuscript. “To better understand how these signals work, we need to know how many active copies of an enzyme it takes to trigger apoptosis in a cell.”
The research team needed to track enzymes known as proteases. These tiny biological catalysts chop up other proteins and have been found to perform many critical cellular functions including the triggering of programmed cell death.

Guy Salvesen, PhD, is professor emeritus at Sanford Burnham Prebys and senior and co-corresponding author of the manuscript. Image credit: Sanford Burnham Prebys.
To trace proteases more directly, the scientists designed new chemical probes that plant a different metallic flag on active or inactive forms of enzymes. These flags can then be analyzed by a machine called a mass cytometer. This single-cell instrument detects metal tags by mass, allowing researchers to count the exact number of enzymes in each state inside individual cells.
“Prior conclusions in the field are largely based on RNA signatures and indirect markers,” said Katarzyna (Kasia) Groborz, PhD, an adjunct faculty member at San Diego Miramar College, former rotation student in the Salvesen lab and first and co-corresponding author of the study.
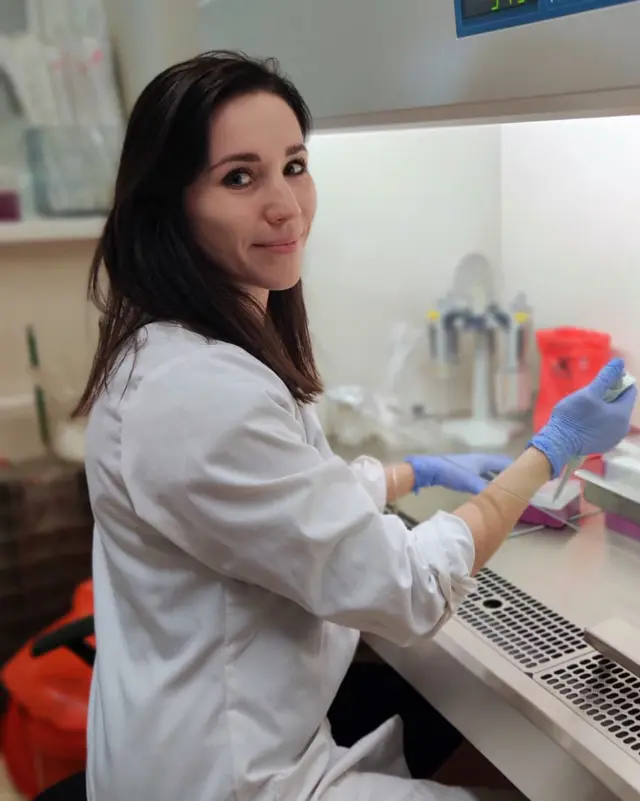
Katarzyna (Kasia) Groborz, PhD, is an adjunct faculty member at San Diego Miramar College, former rotation student in the Salvesen lab and first and co-corresponding author of the study. Image credit: Kasia Groborz.
“This now enables us to correct the fact that there is very little direct mechanistic information about the molecular logic in cells that are dying, such as which enzymes are active and which enzymes decide on the type of cell death that occurs, as well as how all these factors change with disease.”
The researchers tested the new approach on two types of immune cells isolated from healthy blood donors. In white blood cells called neutrophils that defend against infections, the researchers found that individual neutrophils carried considerably different amounts of proteases with varying ratios of active and inactive enzymes. In the case of proteases in the cysteine family, the enzymes remained mostly dormant even in immune cells with higher expression of related genes that were making more copies of these enzymes.
“The data reinforced our conclusion that protease activity is governed after proteins are produced, which limits our ability to infer activity based on abundance as measured by gene expression,” said Salvesen.
In the second set of experiments, the scientists explored how enzyme activity changes as a white blood cell called a monocyte transforms into a more specialized immune cell known as a macrophage. This metamorphosis helps the cellcombat cancer or infection, and now we know it also triggers dynamic changes in protease production and activity.
The research team observed that these adjusted enzyme levels and activity profiles were consistent with the change in function between macrophages and monocytes. Macrophages clamp down on construction and activity of apoptotic enzymes in order to prioritize those linked with inflammatory programs that contribute to the immune system’s response against cancer, infection or injury.
“It’s very exciting for us to be able to describe this because we can now begin to build a much better map of what’s happening in individual cells within a tissue,” said Groborz.
“While we started with immune cells and apoptosis, this is just the beginning and can be applied to other forms of cell death and other diseases,” said Salvesen.
“Ultimately, by revealing what is happening quantitatively at the protein level within individual cells, we hope to provide drug discovery experts with a clear picture of what needs to be blocked or activated to achieve a desired effect to better treat a disease.”
Additional authors include Marcin Poręba and Marcin Drąg from Wroclaw University of Science and Technology.
The study was supported by the National Science Centre in Poland.
The study’s DOI is 10.1016/j.celrep.2025.116810.