Confronting the Threat to Biomedical Research
The NIH’s abrupt decision to cap indirect costs at 15% threatens the future of scientific discovery. This policy endangers research institutions, slows progress and weakens U.S. leadership in life sciences. We stand united in opposition and are actively working to reverse this harmful decision.
Our Impact
At Sanford Burnham Prebys, we bring together visionary scientists, emerging technologies and world-class resources.
In a time of dramatic change in biomedical research, our mission remains steadfast: Turn scientific discovery into a healthier world.


Research Centers
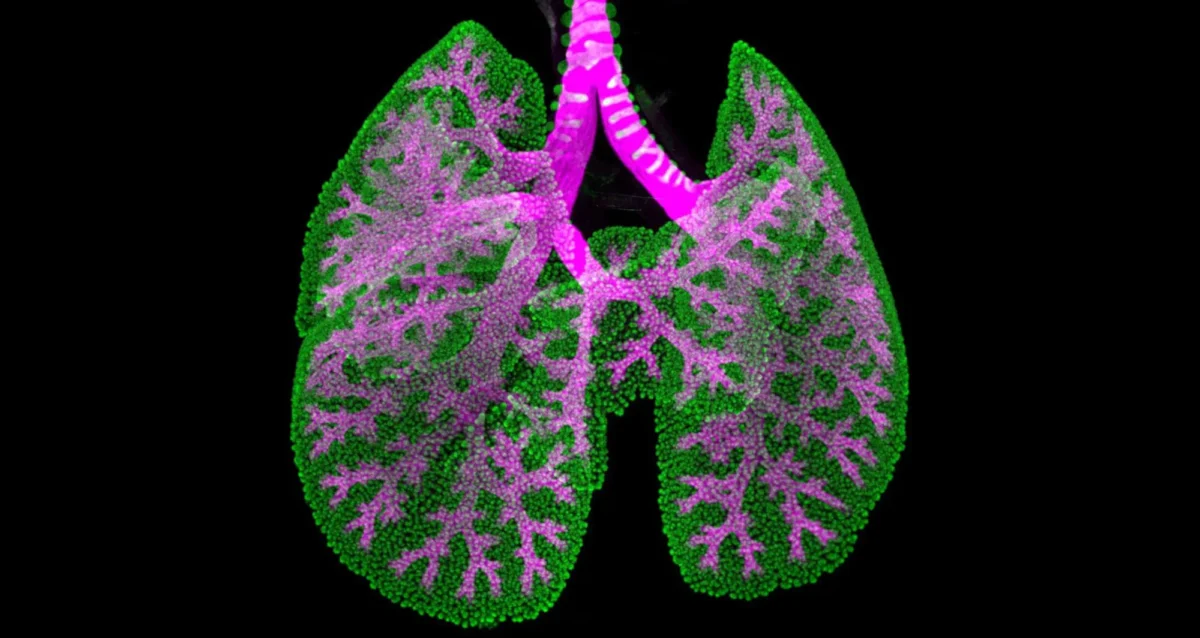
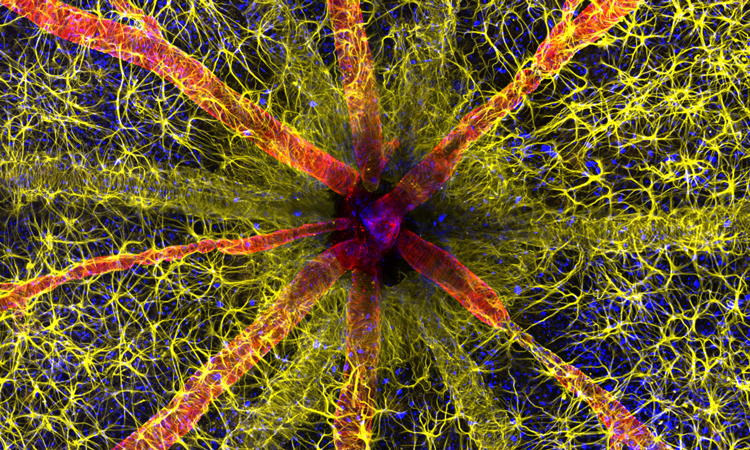
Our four disease-focused research centers target the most pressing health threats: cancer, cardiovascular/muscular, neurologic and metabolic disease. They are supported by three enabling technologies centers for drug discovery, multi-omics and computational biology/artificial intelligence, and enriched by four overarching research themes: aging, immunology/inflammation, stem cells/regenerative medicine and children’s health.

Research Programs
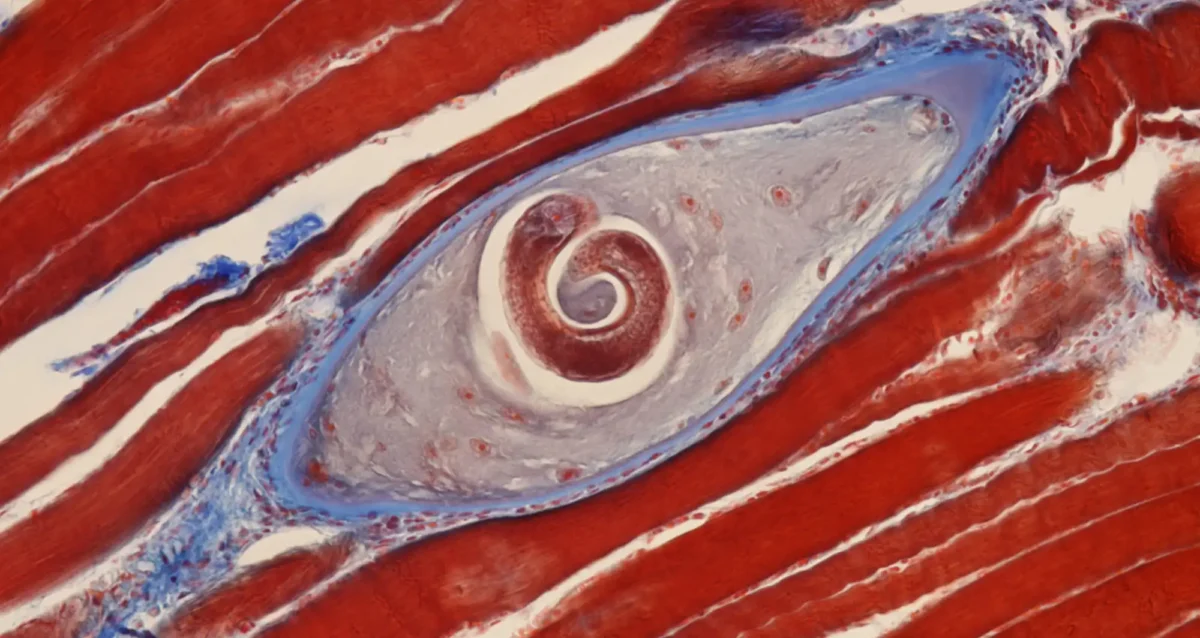
Within the research centers are distinct programs that group together researchers working in key areas of biology to foster collaboration and create a stimulating scientific environment. Programs range from cancer epigenetics to degenerative diseases to aging — and support our work to advance scientific discovery to clinical care quickly and smartly.

Education
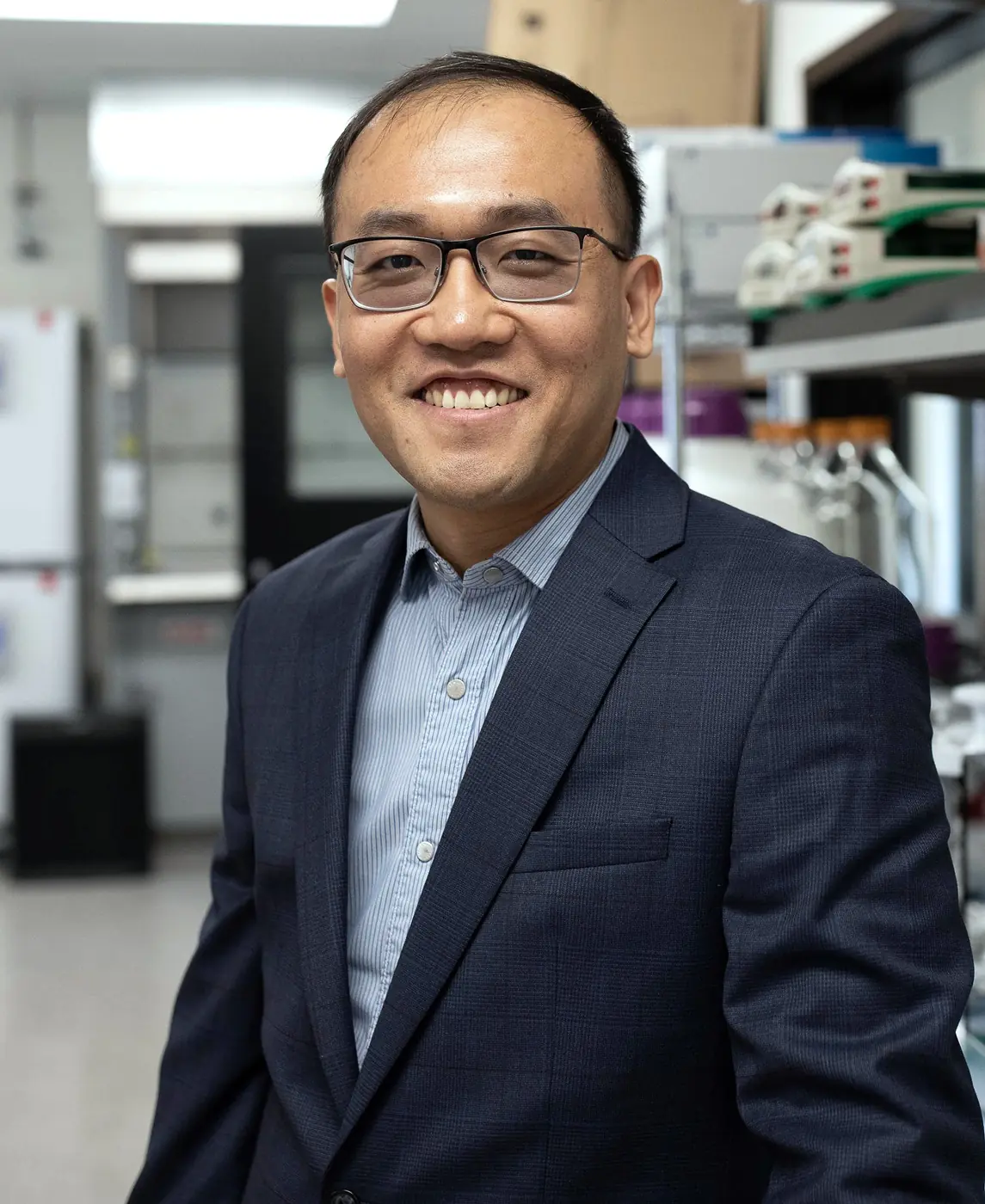
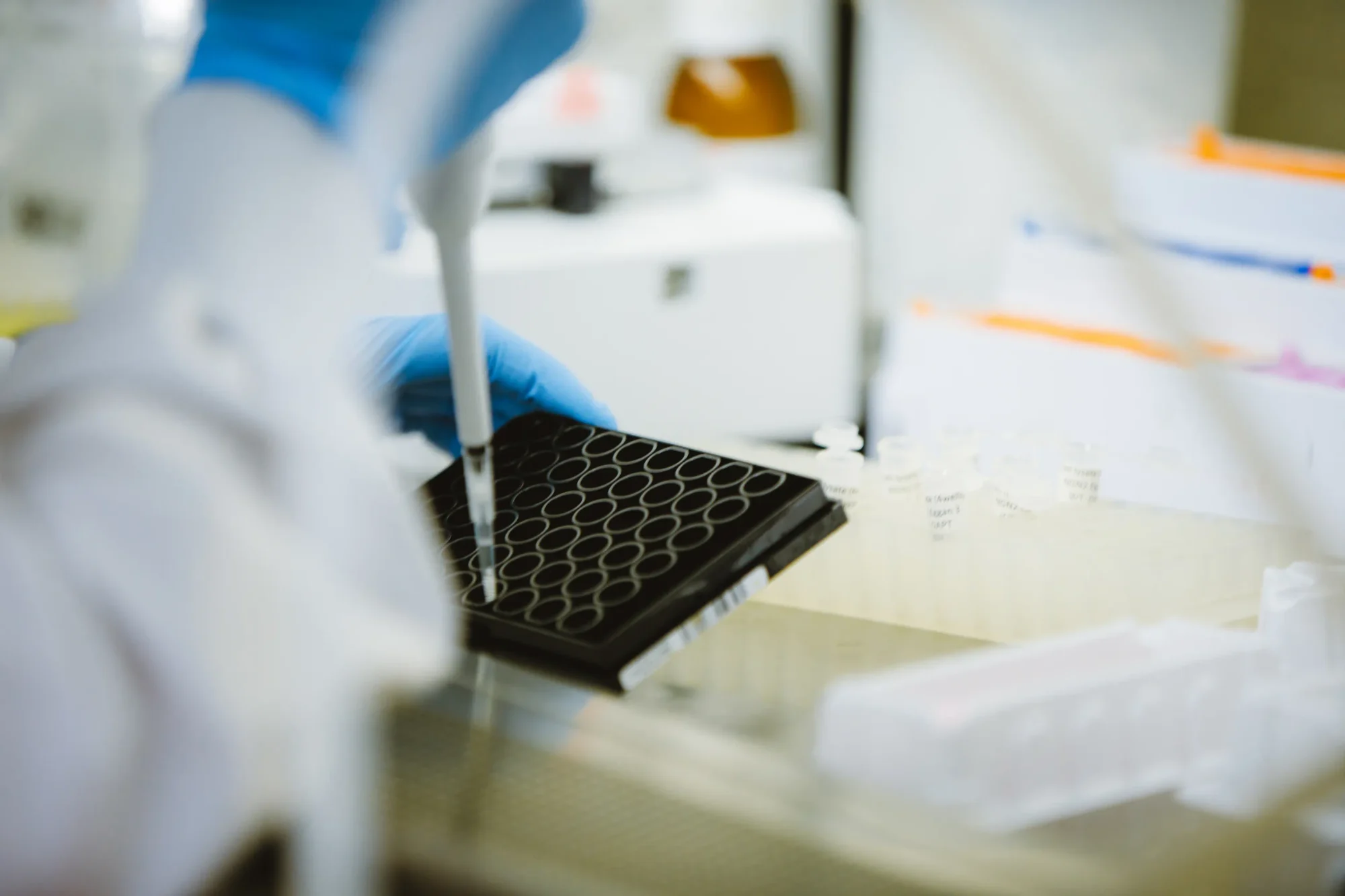
The Graduate School of Biomedical Sciences and post-doctoral programs recruit and train future generations of diverse scientists, combining hands-on laboratory experience with close mentorship from world-class researchers, buttressed by extensive networking and support services.
Our Central Mission
Our four disease-focused research centers target the most pressing health threats: cancer, cardiovascular/muscular, neurologic and metabolic disease. They are supported by three enabling technologies centers for drug discovery, multi-omics and computational biology/artificial intelligence, and enriched by four overarching research themes: aging, immunology/inflammation, stem cells/regenerative medicine and children’s health.
Discovery Driven
Within the research centers are distinct programs that group together researchers working in key areas of biology to foster collaboration and create a stimulating scientific environment. Programs range from cancer epigenetics to degenerative diseases to aging — and support our work to advance scientific discovery to clinical care quickly and smartly.
Science Shaped
The Graduate School of Biomedical Sciences and post-doctoral programs recruit and train future generations of diverse scientists, combining hands-on laboratory experience with close mentorship from world-class researchers, buttressed by extensive networking and support services.