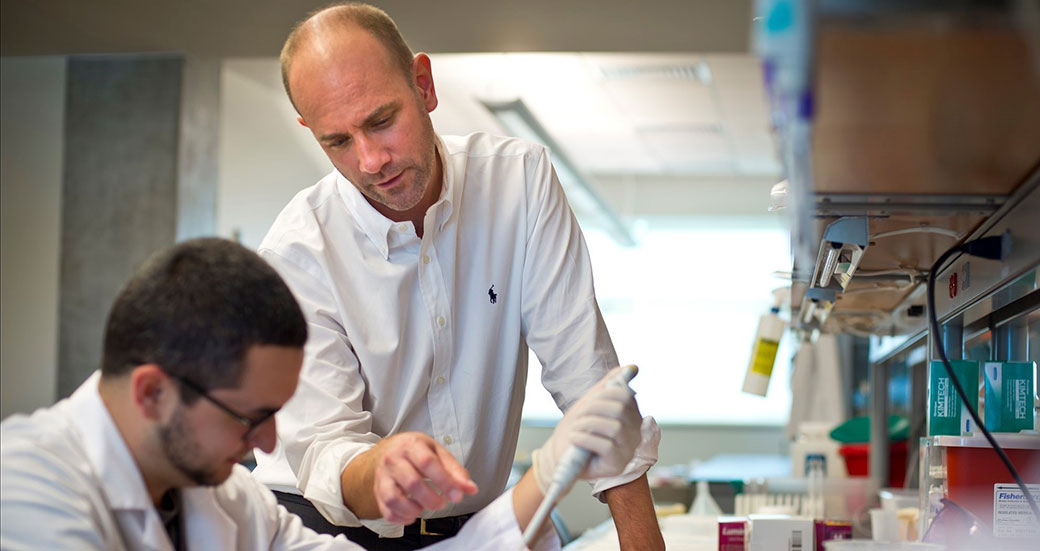
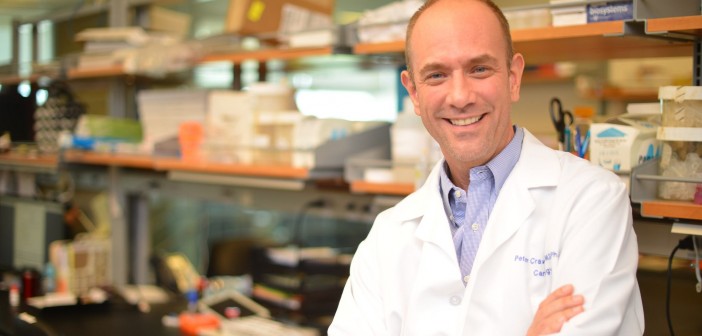
Peter Crawford, MD, PhD, associate professor and director of the Cardiovascular Metabolism Program, and E. Douglas Lewandowski, PhD, professor and director of Cardiovascular Translational Research, have each been awarded R01 grants to continue their pioneering research on metabolic diseases.
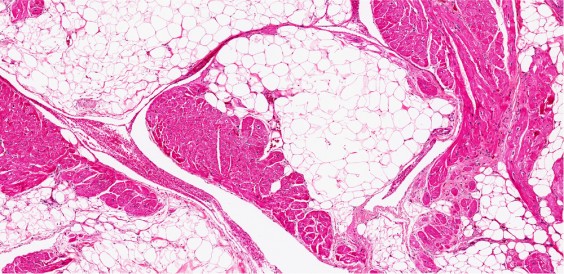
Crawford’s innovative research will investigate whether boosting a type of metabolism called ketogenesis can prevent and treat both non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes. Ketogenesis, which increases when the diet is low in carbohydrates, is the process by which fats in the liver are broken down into small molecules called ketone bodies that can be burned for energy by the rest of the body. Crawford was the first to show that ketogenesis is important even in a normal diet, and is an opinion leader in the field of cardiometabolic research.
“This funding will support our studies to see if ketogenesis can be leveraged as a safe way to eliminate excess calories, even when the carbohydrates are abundant,” said Crawford. “This could lead to a revolutionary type of therapy for these epidemic disorders.”
NAFLD affects approximately one billion individuals worldwide and has become a leading cause of cirrhosis, which can lead to liver cancer. Type 2 diabetes is a similarly enormous public health problem, as almost 400 million people have the condition, often only diagnosed after complications arise, such as nerve damage, kidney problems, and vision loss. Both diseases increase the risk of heart attacks and stroke.
The second grant will support Lewandowski’s lab in studying fatty acid metabolism in heart failure, the condition in which the heart cannot pump sufficient blood to supply the body with oxygen. He is preeminent among investigators who focus on the metabolic basis of this form of heart disease.
Heart failure, which can severely limit patients’ ability to complete day-to-day tasks, impacts more than 23 million people globally. While management of this condition is improving, only 50% of patients will survive five years after diagnosis.
Lewandowski has previously shown that as the heart progresses toward failure, it becomes inefficient in utilizing fuels, like fats and carbohydrates. He was the first to demonstrate the appearance of a key protein that is expressed genetically during progression of heart failure to alter how fats are oxidized. His new grant will enable the lab to target this enzyme with therapeutic protocols to potentially reverse the decline in energy available for the pumping ability of diseased hearts. He also recently demonstrated that oleate, a common dietary fat found in olive oil, restores proper metabolism and enhances pumping power in an animal model of heart failure, and the new grant will further the investigation of how certain dietary fats affect diseased hearts.
“We will examine the cellular events underlying oleate’s effects,” said Lewandowski. “We’re confident that this will lead to new therapeutic targets to preserve heart function. This would fill a pressing need, as no current treatments directly interfere with the mechanisms that cause progressive damage to heart muscle.”