This post was writing by Kelly Chi, a freelance writer.
New research shows the uniqueness of a promising technology that SBP scientists are employing to deliver large payloads of drugs to tumors. The findings, published recently in the journal Science Advances, not only lend insight into how large molecules get into cells, but also show how a compound the team previously discovered may work to target cancer cells.
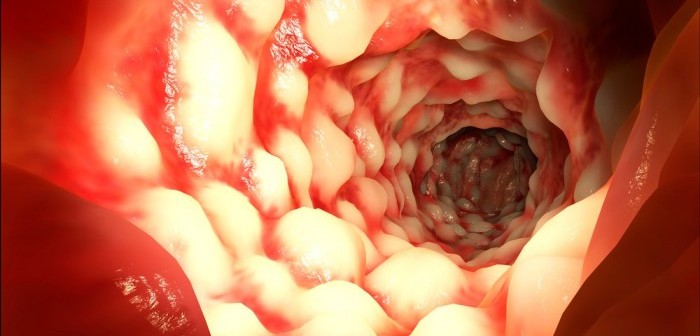
One main challenge in treating cancer is delivering sufficient amounts of drug to the intended target. Often, cancer drugs do not penetrate the tumor but instead hit only a few cells. Surviving cells proliferate, and those given only a small dose can evolve resistance to treatment.
Erkki Ruoslahti, PhD, distinguished professor in SBP’s Tumor Microenvironment and Metastasis Program, and his team at SBP have been hunting for small-protein drugs that make drugs do a better job at penetrating tumors. The way the scientists do this is to inject an entire ‘library’ of different small proteins (or peptides) into mice with cancer, and see which ones, if any, reach the tumor.
More than a decade ago, they found a unique peptide that took only minutes to reach the tumor after being injected into the bloodstream.
Only later, in 2009, having discovered another peptide, iRGD, which had similar properties, did they find out what made these peptides special. They included a short string of amino acids in a particular pattern that gave it the ability to penetrate tumors. The pattern, called CendR, has been a major focus of Ruoslahti’s research.
“The iRGD peptide was special because by using it we could get a drug to go deeper into a tumor and hit all the tumor cells, not just the ones that are close to the blood vessels, which is usually what happens,” said Ruoslahti.
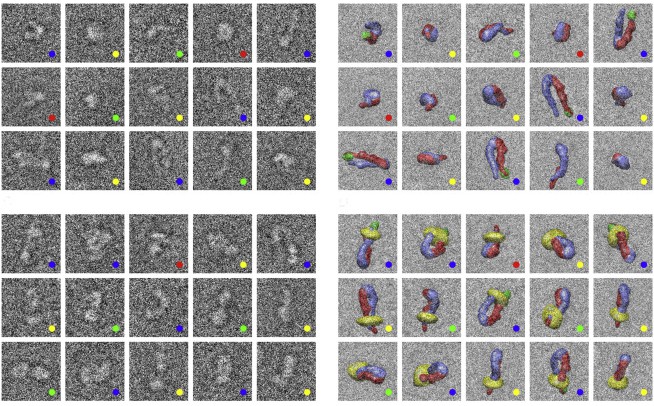
Last year, the group learned even more about iRGD. In Nature Communications, they showed that the peptide triggers a unique mode of transport into the cell, unlike what has been seen before. It does so by binding to a receptor on the cell surface called neuropilin1, which is itself involved in crucial functions, including the movement of fluid and other molecules across walls of blood vessel cells.
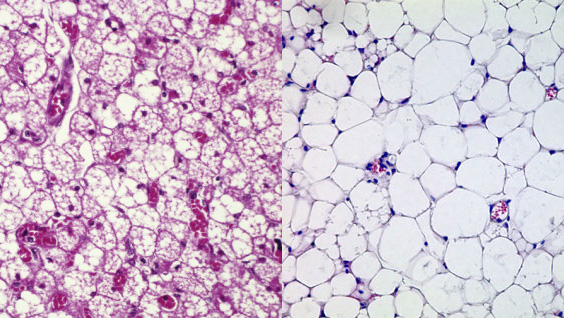
There are many ways that molecules can get into cells. iRGD appears to trigger cells to swallow large vesicles. This process is similar to a mechanism known as ‘macropinocytosis’ (macro meaning ‘large’; pino ‘drink’; and cyte ‘cell’) yet distinct in some ways, Ruoslahti said.
In the new study, the research team did additional work to characterize CendR’s actions, comparing them with another known peptide technology (TAT) that is often used to get drugs into cells.
“That pathway [TAT] is not specific for tumors and can’t be made specific for tumors as ours can. That’s one difference, and we show other differences between the two pathways in this paper,” Ruoslahti said.
Another key feature of the CendR pathway is that it’s affected by the nutrient status of the tissue.
“If the tissue, in our case a tumor, is deficient in nutrients and needs more, it activates the pathway, which fits perfectly with the idea of why this pathway exists: it brings in nutrients. In contrast, TAT is not affected by nutrient status, so it probably has another function.
“We turn on the pathway with iRGD only in the tumor, not in normal tissues. At the same time, we slip a drug into the pathway as a stowaway, and the result is that more of the drug accumulates in the tumor than would get there otherwise, and the drug also penetrates deeper into the tumor. These features make iRGD promising as an adjunct to various kinds of chemotherapy,” adds Ruoslahti.
The iRGD peptide is undergoing preclinical development, namely mouse toxicology studies that are needed before the team can apply to investigate it in humans. The team has another year’s worth of work ahead. But they already have reason to believe that iRGD might work: it binds to the human version of its receptor. In addition, they have seen promising results after testing the peptide in tumor tissue from people with cancer.
Other authors on the paper are staff scientists Hongbo Pang, PhD, and Gary Braun, PhD, both of SBP.
The full paper can be found at: http://advances.sciencemag.org/content/1/10/e1500821