In the last 12 months, SBP scientists published 338 scientific papers—that’s almost a paper a day. We are proud of this impressive achievement, and equally proud of the quality of research in these scientific studies. Whether you are seeing them for the first time or coming back for another look, check out the most popular stories from SBP’s researchers in 2017.
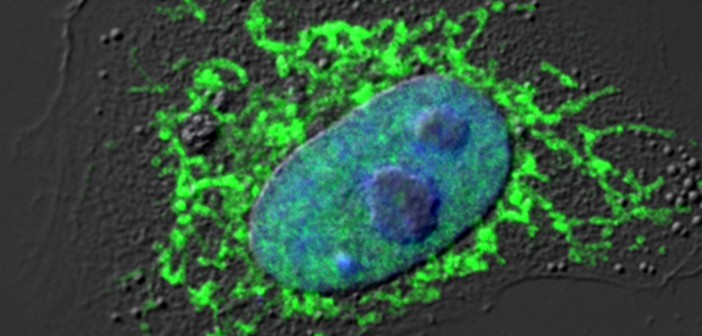
- Scientists take a deeper dive into cellular trash
Malene Hansen, PhD, led the first-ever comprehensive analysis of autophagy in a living animal during aging. The study was published in eLIFE. - Drug short-circuits cancer signaling
A drug that zeroes in on mutated nuclear receptors found in cancer will soon be entering Phase 1 clinical trials at the Dana Farber Cancer Center for patients with colorectal cancer. Research by Xaio-kun Zhang, PhD, describes how the targets cancer but leaves normal proteins alone. - Biomarker may predict early Alzheimer’s disease
Erkki Ruoslahti, MD, PhD, has discovered a new approach to detect Alzheimer’s disease at its earliest stages. His research team found a biological marker, or biomarker, that’s associated with brain inflammation—a trigger for the Alzheimer’s process, which takes many years to produce symptoms. - Steps toward a promising therapy for a rare bone disease
Yu Yamaguchi, MD, PhD, led a study proving fresh insight into the mechanism of multiple hereditary exotoses (MHE)—a rare disease that causes the growth of multiple benign bone tumors. The research opened the door for testing the drug palovarotene in Phase 2/3 clinical trials for patients with MHE. - New insights into bipolar disease
An international collaborative study led by Evan Snyder, MD, PhD, was first to explain the molecular basis of bipolar disease and may support the development of a diagnostic test for the disorder. The research may also help scientists develop tools to predict the likelihood of patient response to lithium treatment—a highly effective drug that works in only 30% of bipolar patients.