Rare but deadly condition begins with metabolic changes to make a pro-fibrotic metabolite.
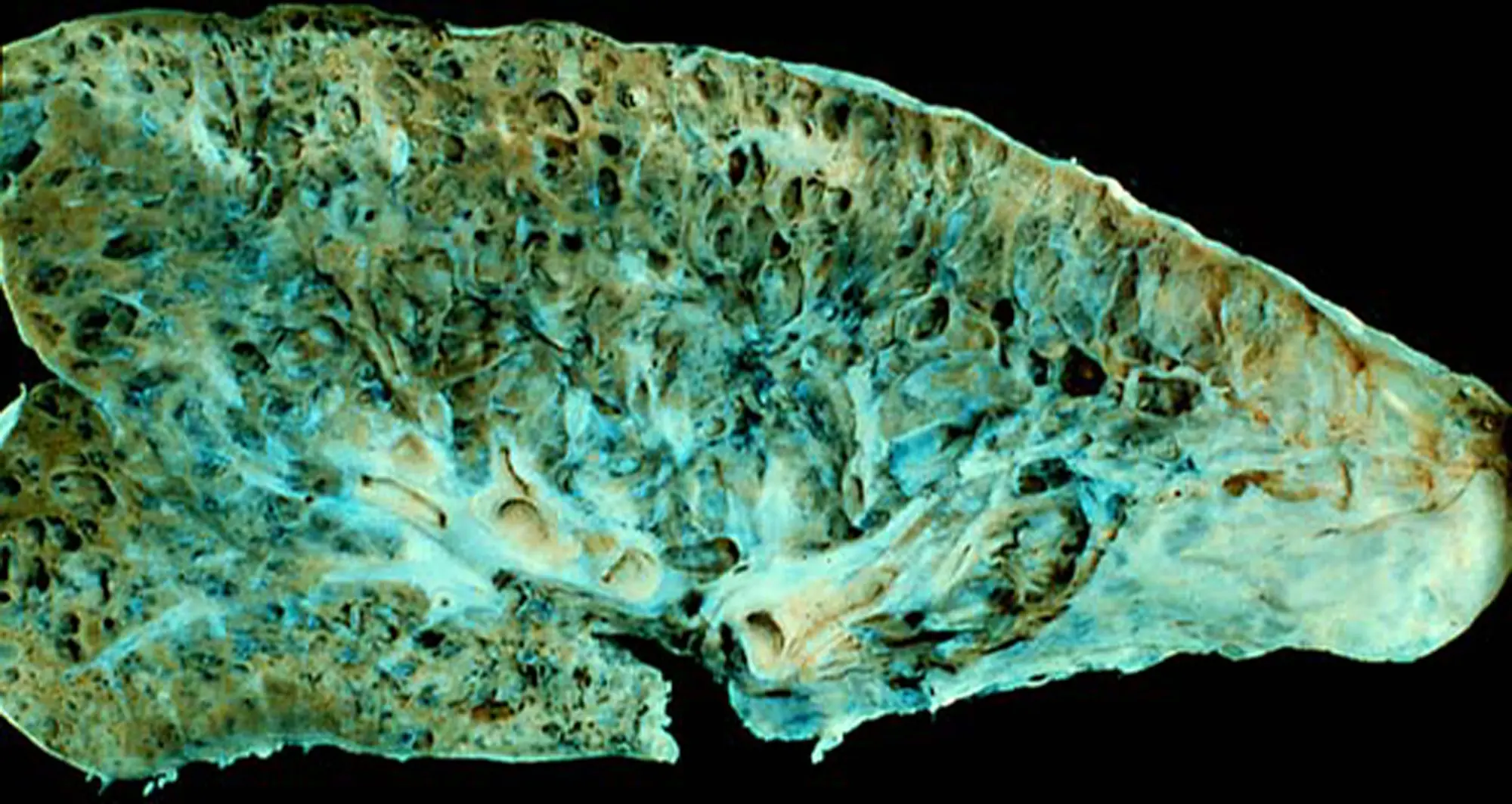
Idiopathic pulmonary fibrosis (IPF) is an irreversible disorder of the lungs, characterized by gradual, chronic scarring of alveoli — the tiny, balloon-shaped air sacs where oxygen and carbon dioxide are exchanged with circulating blood.
The symptoms and consequences of IPF are well-known (progressive loss of lung function), and dire. Though there are treatments to slow disease progression, there is no cure. Median survival time after diagnosis is three to five years.
While gender, genetics and behaviors like smoking are risk factors, the exact cause of IPF is not known. In a new paper published in The Journal of Clinical Investigation, an international team of scientists, including Kevin Tharp, PhD, assistant professor in the Cancer Metabolism and Microenvironment program at Sanford Burnham Prebys Medical Discovery Institute, posit the beginnings of an answer, describing how crosstalk between myeloid cells (immune) and fibroblasts (a mesenchymal cell type that is ubiquitous throughout the body) drives inflammation-induced overproduction of collagen (fibrosis) in lung tissues.
Using murine models of disease and human samples, Tharp and collaborators (including senior author Mallar Bhattacharya, MD, associate professor of medicine at UC San Francisco), showed that ornithine, a non-protein amino acid produced by myeloid cells expressing the gene Arginase 1 (ARG1), serves as a pro-fibrotic metabolite that drives the overproduction of collagen in the lungs by neighboring fibroblasts.
While these findings increase understanding of metabolic contributions to the disease, said Tharp, the importance of this work lies in the revelation that IPF may be treatable with diet and small molecule drugs.
The findings suggest the molecular basis for new treatments that target ornithine production to stop disease progression in IPF patients, Tharp said. Even though the predominant ARG1-expressing myeloid cells in mouse lung models were macrophages and ARG1 was primarily expressed in human neutrophils, a related immune cell type, the metabolic program required to overproduce collagen is the same.
The findings build upon work published in 2024 in the journal Nature Cancer.

In that research, Tharp, with colleague Kelly Kersten, PhD, an assistant professor in the Cancer Metabolism and Microenvironment program at Sanford Burnham Prebys, and others, describe how metabolic behavior of macrophages contributes to the thick layer of fibrous collagen called tumor-associated fibrosis, which is thought to act as a barrier to infiltrating anti-tumor immune cells, such as cytotoxic T lymphocytes (CTLs).
Specifically, they found that in breast cancer, tumor-associated macrophages (TAMs), a type of immune cell found abundantly in the tumor microenvironment, drive progressive fibrosis by producing ornithine and injury-associated collagens that facilitate wound closure and “re-epithelialization”.
The metabolic changes in TAMs facilitate the overproduction of ornithine from arginine through the action of ARG1. Tharp and colleagues found that when macrophages produce ornithine, used to synthesize collagen, they can also suppress the anti-tumor function of CTLs, creating even more of challenge for anti-tumor responses than the physical barrier.
“CTLs normally migrate through spaces much smaller than the gaps in collagen networks that form around tumors,” Tharp said when the paper was published. “Our study provides an alternative explanation for why anti-tumor immunity is impaired in fibrotic solid tumors.”
“Taken together, these two papers show that fibrosis is dependent on a new metabolic circuit that is orchestrated by ARG1 expressing immune cells that metabolize amino acids into ornithine, which is a pro-fibrotic metabolite,” said Tharp.
“Dietary changes that limit the abundance of ornithine and small molecule inhibitors that prevent its production or excretion are likely effective therapeutic strategies to reduce the severity of fibrotic disease in many tissue and tumor types.”
Mallar Bhattacharya of the University of California San Francisco is senior author of the JCI paper; Preeti Yadav, also at UCSF, is first author.
Additional authors include:
Javier Gomez Ortega, Nivedita Biswas, Aritra Bhattachraryya, Kaven Boostanpour, Tanay Jujaray, Jasper T. Wang, Tatsuya Tsukui, Christopher J. Molina, Vincent C. Auyeung, Dean Sheppard, Mazharul Maishan, Hiroki Taenaka, Michael A. Matthey, Paul J. Wolters.
Prerna Dabral, Satish K. Pillai, Whitney Tamaki, Trever G. Bivona, Charles Chien, Allon Wagner, Kai-Chun Chang, Sixuan Pan, Adam R. Abate, Julia Nilsson, Ari B. Molofsky, Xiaoyang Yin, Baosheng Li, Rieko Muramatsu, Lenka Maliskova, Arnab Ghosh, Walter L. Eckalbar and Stanley J. Tamaki, all from UCSF.
The study was supported by funding from the US Department of Defense, the UCSF Bakar Aging Research Institute), Longevity Impetus Grants from Norn Group, a UCSF Bakar Aging Research Institute investigator award, the Nina Ireland Program for Lung Health Innovative Grant Program and the National Institutes of Health.
The study’s DOI is 10.1172/JCI188734.