He doesn’t need money to produce an album. He’s not raising funds to start a new business in his hometown. And he’s not asking for cash because he’s a famous rapper who suddenly finds himself “bankrupt.” He is a young scientist who needs money to conduct research aimed to save lives, so he is turning to crowdfunding.
Joseph Lancman, PhD, is a scientist in the organogenesis lab of Duc Dong, PhD, at Sanford Burnham Prebys Medical Discovery Institute (SBP) in La Jolla. Lancman’s crowdfunding site just went live on Diabetes Research Connection (DRC), a San Diego-based company that created a platform to connect donors directly with early-career scientists. In the next 90 days, Lancman hopes to generate $50,000 for his research project that may provide the scientific breakthrough needed to find a cure for type 1 diabetes. Watch his video here.
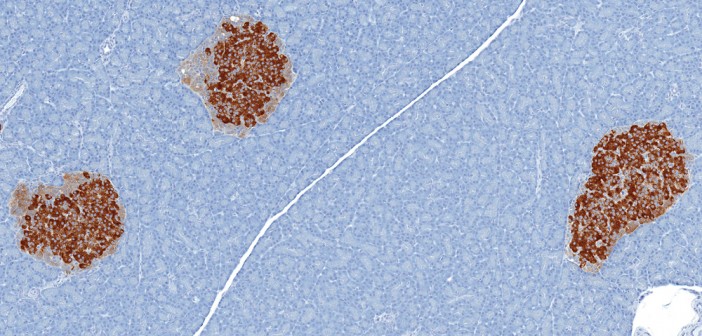
“We recently discovered a way to reprogram cells and change their identity without removing them from the body,” Lancman said. “We believe this breakthrough will have great implications for people with degenerative diseases, like diabetes.”
As many as three million Americans have type 1 diabetes. Millions of children and adults struggle with this disease, yet funding has decreased dramatically for research. In fact, the head of the National Institutes of Health (NIH) said last year that young scientists in this country now face the worst funding in 50 years.
So, if you are a young scientist with a great idea, where do you go? Alberto Hayek, MD, co-founder and president of the DRC and world-renowned diabetes expert, says some go away. “Due to the limited funding available, scientists just starting out in their career are forced to leave the field of diabetes and go to fields that have more funding. We are giving scientists the funding needed to test and validate research that departs from conventional thinking,” Hayek said.
Dong says his lab heard about DRC from others in the field. “The DRC is committed to funding innovative projects that may not be considered mainstream approaches. The crowdfunding model itself is highly innovative, by making sure that 100% of donations will go directly into specific labs and projects chosen by the individual donors,” Dong said.
And it works. Since DRC launched its platform in 2014, six research projects from all over the country have been 100% funded. Every dollar of the money raised goes directly to the scientist. The power to fund projects has been given to the people.
Lancman has a total of 90 days to make it happen. He needs 5,000 people to donate $10 each in order to reach his goal. He’s excited to be able to continue to work towards a cure for diabetes, and allow people to live full lives without painful daily insulin injections.
Come on, social media.