From how much coffee we can tolerate to the amount of weight we can lift, our bodies differ from one another in myriad ways. But when it comes to medicine, historically every patient with the same disease or condition has received the same treatment—even though individual responses vary wildly.
Now, technological advances are enabling medicine to move from “one size fits all” to tailored treatments based upon one’s specific genes. This approach is called precision medicine.
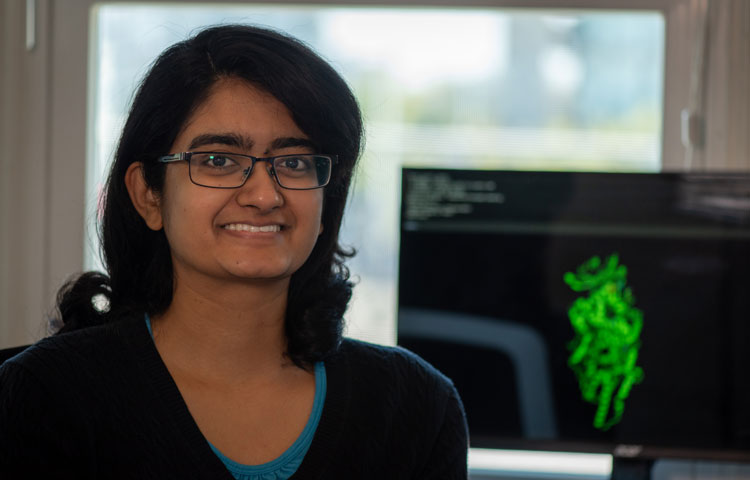
This December, under the dome of the Fleet Science Center’s IMAX theater, Jessica Rusert, PhD, a postdoctoral researcher in the lab of Robert Wechsler-Reya, PhD, explained the promise and potential of precision medicine to a crowd of nearly 100 people as part of the museum’s Senior Monday presentation series (if interested, check out the 2019 schedule).
We caught up with Rusert to learn more about the goals of precision medicine and her work in the Wechsler-Reya lab.
Before the advent of precision medicine, how did doctors typically treat patients?
In the past, all patients who had the same disease—say, breast cancer—received the same treatment, which was most likely surgery followed by chemotherapy and radiation. Your treatment might change if you have more advanced disease—in which case the approach would be more aggressive. But typically treatment was based upon physical criteria: the location of the tumor, your symptoms or how the tumor looks under a microscope. That’s not to say this is a bad approach; it was simply the only information doctors and scientists had to work from.
What catalyzed the movement from one size fits all to personalized treatment?
The invention of DNA sequencing has revolutionized personalized medicine. As the cost of sequencing decreases and the use of the technology swells, we will glean even more information from the genome, and personalized medicine will expand further to new areas.
What is the ultimate goal of precision medicine?
Precision medicine aims to treat the right patient, with the right drug, at the right time.
How far away is precision medicine from this goal?
We are making inroads, but it is still early days for precision medicine. Currently, we are making the most progress in cancer. But despite these advances, the vast majority of cancers—including the pediatric brain cancer our lab studies—are treated with surgery, chemotherapy and radiation.
As scientists learn more about the underlying cause of disease(s), precision medicine will expand to new cancers and new disease areas. These advances are happening now, and for some cancers, the outlook is already much better than it used to be. Perhaps one day we will have personalized treatments for schizophrenia and autism. The approach is mostly limited by how much we know about a disease.
What is an example of a precision medicine?
The breast cancer treatment Herceptin® is a great example of a precision medicine.
Cells in our body use molecular antennae called receptors to sense and respond to their environment. One receptor, called HER2, controls cellular growth, and is involved in the development of breast cancer.
Herceptin works by blocking the HER2 receptor. Then, the receptor can’t tell cells to grow, and tumor growth stops.
However, this medicine only works if your tumor cells have this receptor. HER2-positive breast cancer means your cells have this receptor. HER2-negative breast cancer means you do not have the receptor, and thus Herceptin wouldn’t work for you. So people with breast cancer are tested to ensure they have the HER2 receptor before receiving Herceptin.
Herceptin has saved thousands of lives. It is a true testament to the power of precision medicine.
What was a popular question from the audience?
A lot of people wondered if there’s a way to prevent cancer. This is understandable—cancer is scary, and we want to do all we can to stop it. But it’s a difficult question to answer. The science isn’t there yet. We are only just now starting to understand how to help people who have acute disease. We may understand how to prevent cancer one day—but that will take decades, not years.
How do you use precision medicine in your work?
In the Wechsler-Reya lab, we are working to find personalized treatments for children with brain cancer. We are studying the most common malignant pediatric brain cancer, called medulloblastoma.
Children with medulloblastoma undergo surgery to remove the tumor and then undergo chemotherapy and radiation treatment. This treatment is hard for adults to go through—and even more devastating for a developing child. The treatment leaves long-term effects, including cognitive impairment and increased risk of other cancers due to the DNA damage caused. A treatment that reduces or eliminates these side effects is urgently needed.
Scientists are learning that medulloblastoma is not one cancer, but actually four clearly defined subgroups. We are working to better understand these subgroups so we can develop targeted treatments that are customized to each cancer type (read the lab’s recent discovery).
Where is precision medicine heading in the future?
Right now, most precision medicine focuses on our DNA, but there are many other ways we differ from one another. But increasingly, scientists are working toward precision medicine that also takes into account RNA, proteins, our metabolism, the epigenome (molecular tags on DNA) and more.
Interested in keeping up with SBP’s latest discoveries, upcoming events and more? Subscribe to our monthly newsletter, Discoveries.