As an infectious disease immunologist studying Lyme disease, Victoria Blaho is one of a rare breed.
Sanford Burnham Prebys assistant professor Victoria Blaho, PhD, investigates the biochemical signals of the immune system and how they impact our bodies’ abilities to fight pathogenic infections, a branch of immunology that has become much less popular since the advent of antibiotics in the early 20th century.
Blaho’s disease of choice is Lyme disease, an unusual tick-borne bacterial infection that affects some 476,000 people in America each year, a number that is on the rise.
We caught up with Blaho to talk about why Lyme disease research is important, the progress being made and the work that remains in studying this strange and burdensome disease.
Why is Lyme disease research important?
Blaho: Lyme research is a very small field for a disease that is becoming bigger and bigger every year. Case counts are increasing for Lyme disease all over the world, and people get very sick from it. Some people are infected, take antibiotics and that’s the end of it. But others have chronic symptoms like arthritis or carditis that can last for years and become completely debilitating.
What makes Lyme difficult to study?
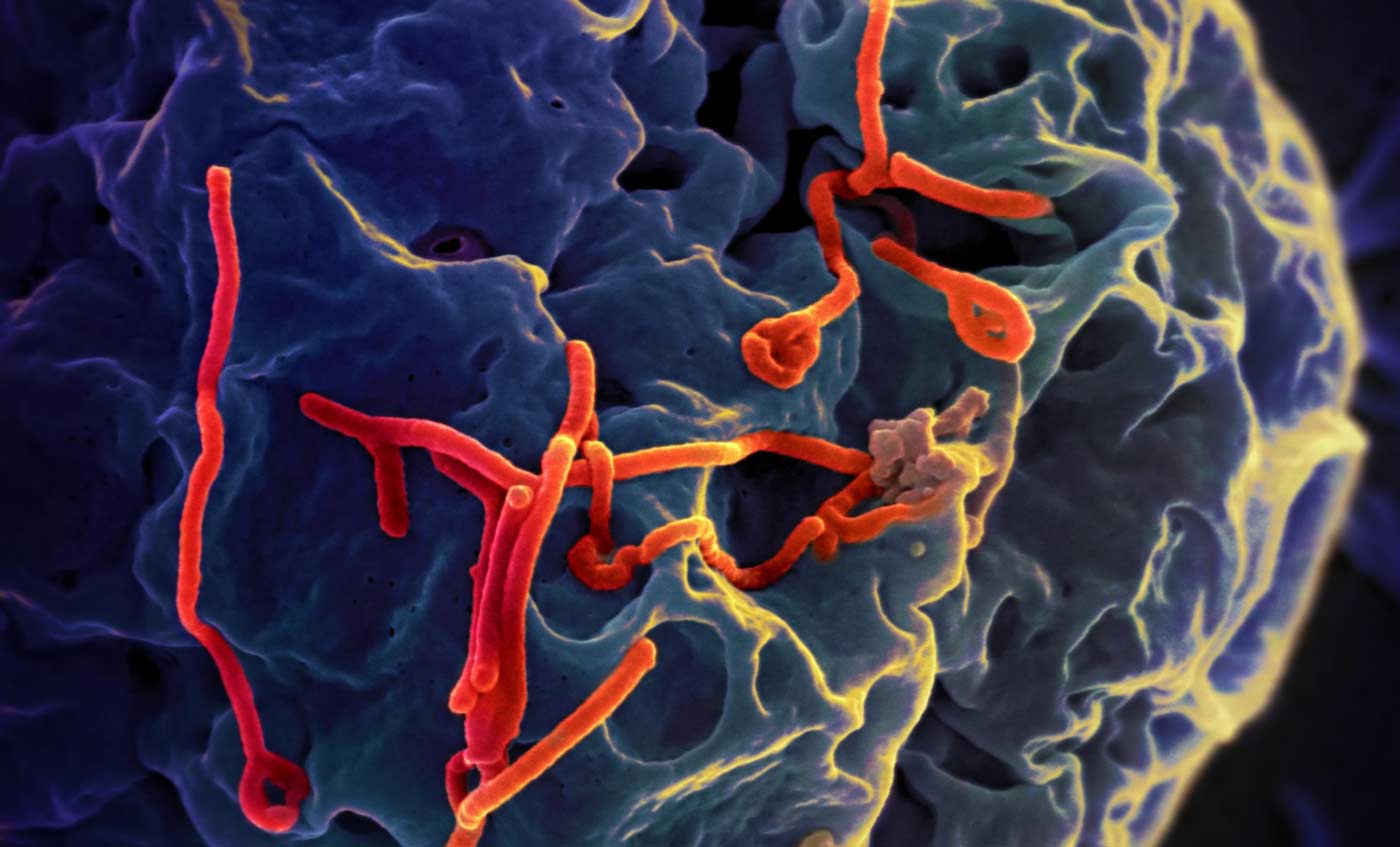
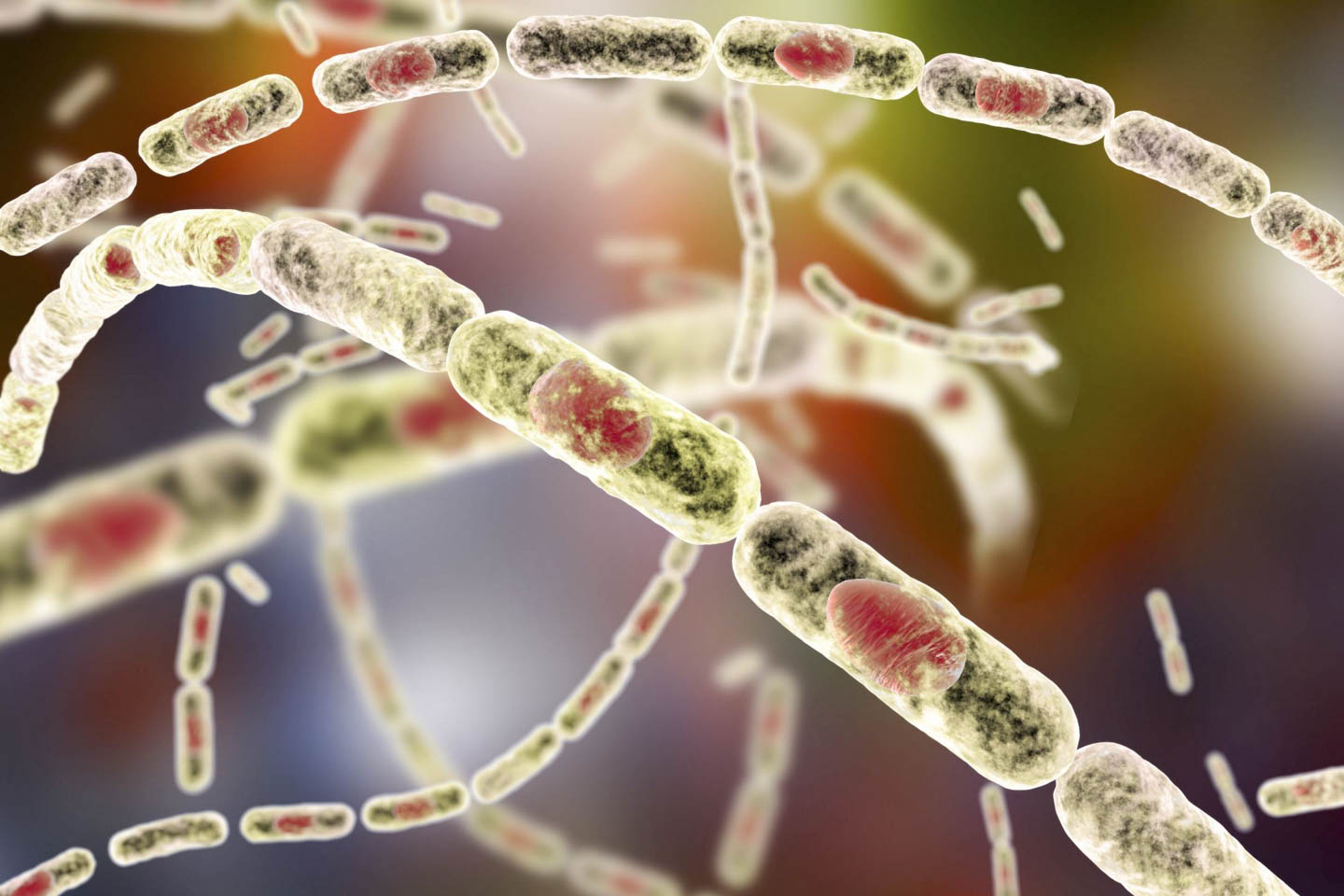
Blaho: One reason is that Lyme is an unusual infection from a microbiological standpoint. In the early days of Lyme research, there were studies showing that the bacteria that caused the disease, Borrelia burgdorferi, could change its physical form from a corkscrew shape to dormant blobs—and the blobs could be causing extended disease. This is a problem because scientists haven’t agreed on the true cause of chronic Lyme disease.
To make matters worse, a lot of the medical field still believes Lyme is easily curable with antibiotics, and if people are still having problems, then it’s psychosomatic. This makes it harder to get support for research into the longer-term inflammatory effects of Lyme. These politics make Lyme disease research a strange ecosystem of patients, physicians, researchers and funding agencies, and this is a barrier to learning more about the disease and helping people find relief.
How does your work enter the picture?
Blaho: I’ve been working on Lyme disease for over 15 years, since I was PhD student. It started because Celebrex was hugely popular at the time to treat arthritis, but nobody had ever studied it in the arthritis that emerges in Lyme disease. Celebrex inhibits an enzyme of the immune system that triggers inflammation, so we figured that Celebrex might work just as well in Lyme arthritis as in other types. But research on mice didn’t bear this out.
Inflammation doesn’t just peter out when an infections clears. The immune system has to clean up the mess. We discovered in mice that Celebrex inhibits the resolution of inflammation after Lyme disease has resolved, so the arthritis never went away.
Since then, my career has focused on exploring the signaling molecules that regulate inflammation and its resolution. These molecules affect all parts of the immune system and provide us with a whole host of different potential therapeutic targets for inflammatory diseases like chronic Lyme.
What are the next steps for your Lyme research and for the field at large?
Blaho: My own immediate next step is to take the work I’ve been doing here at Sanford Burnham Prebys and connect it directly back to my original work with Lyme. My team here is currently working on a signaling molecule called S1P, and while we haven’t studied it in Lyme yet, we think there are connections between it and the immune mediators we first found through those Lyme studies.
Our next steps are to look for the protein that carries S1P in mice with Lyme disease. This protein is associated with disease susceptibility in other inflammatory illnesses like diabetes and cardiovascular disease, and we think it has a role to play in Lyme as well. We’re also planning to partner with the Bay Area Lyme Foundation to see if we can find changes in this protein in their collection of human samples.
More broadly, I think this field is hungry for innovation because there have been a small number of scientists focusing on it. If older ideas about Lyme being simple to treat were the complete picture, we’d already be able to better diagnose and treat patients. But we’re just not there yet.
Lyme may be a lot cleverer than we originally thought, but if we’re able to embrace new technologies and ideas and continue to push forward with new work, we’ll be able to find innovative approaches to fight Lyme and, ultimately, to help people suffering from this horrible disease.