Few cellular systems are more important than mitochondria. These organelles convert the body’s fuels into ATP, the biological energy packets that power many of the cell’s most important functions. Mitochondria are especially important in the heart and other muscles, which use a lot of energy.
Needless to say, impaired mitochondria could have a major impact on health, making them an intense area of study in the biomedical community. Daniel Kelly, M.D., scientific director at SBP’s Lake Nona campus, recently collaborated with investigators at Washington University to better understand how heart mitochondria are built after birth.
“During fetal development, the heart does not have huge energy requirements,” notes Dr. Kelly. “But after birth, it has to pump blood throughout the body—and that takes a tremendous amount of energy. To equip itself, the heart has a virtual explosion of mitochondrial biogenesis after birth.”
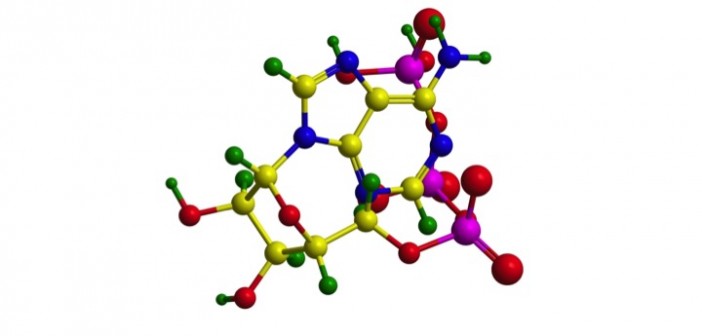
A few years ago, Dr. Kelly’s lab showed that a group of proteins called PGC-1 coactivators drive this mitochondrial population explosion. But in the new study, led by Washington University researcher Gerald Dorn, MD, and published in the journal Science, the team showed that it’s not enough to just add new mitochondria; heart cells must first remove older, fetal mitochondria, a process called mitophagy. Fetal mitochondria just aren’t well-suited for this new role.
“During the fetal period, heart mitochondria largely use glucose,” says Dr. Kelly. “But after birth they switch to multiple higher octane fuels, particularly fatty acids. You have to wipe out the fetal mitochondria and build new mitochondria that are capable of using fatty acids.”
In the study, the researchers suppressed mitophagy in mice shortly after birth by preventing a protein called Parkin from driving this important quality control function. They found that, without clearing old mitochondria, new ones were not produced, dramatically impacting heart size and function.
Dr. Kelly’s lab and Lake Nona’s metabolomics facility played a major role in the research, providing expertise on mitochondria and measuring the compounds produced by mitochondria to track their function. The adult metabolomics signature did not occur when mitophagy was prevented. This study provides great insights into mitochondrial adaptability and could illuminate better ways to treat adult disease conditions.
“Although it’s early days, this work has profound implications for diseases related to mitochondrial dysfunction, such as heart failure, diabetes, and neurological conditions,” says Dr. Kelly. “It’s possible that under stressful conditions, such as a heart attack or high blood pressure over long periods, the body calls on this quality sorting mechanism again to adapt. Future studies will address this question.”
This post was written by Josh Baxt, a freelance writer.
To read the paper click here