The new project will help researchers better understanding why current gene therapy treatments aren’t working.
A multi-institute research collaboration including Sanford Burnham Prebys has just received a $12 million grant from the National Heart, Lung, and Blood Institute to improve hemophilia therapy. The award will fund three projects that could lead to safer and potentially curative treatments for the disorder. One of these projects will be led by Randal J. Kaufman, PhD, who directs the Degenerative Diseases Program at Sanford Burnham Prebys.
How viruses could be help treat hemophilia
Hemophilia is an X-linked genetic condition that prevents the blood from clotting properly. It occurs in about one out of 5,000 male births. In patients with severe forms of the disease, internal or external bleeding can be life threatening. Standard treatments for severe hemophilia involve intravenously replacing the clotting proteins that patients are unable to produce adequately on their own. However, a gene therapy approach uses viruses as a delivery mechanism to provide the body with the information it needs to start making its own clotting factors.
“Several companies have taken this forward into clinical trials, and in some of these trials, the patients initially looked like they were cured,” says principal investigator Roland W. Herzog, PhD, the Riley Children’s Foundation Professor of Immunology at Indiana University School of Medicine. “But what they all have in common is that they need to deliver a lot of the virus in order to get the desired results, and over time, clotting factor levels started to decline. So it’s clear that we need to further study the biology of this phenomenon.”
How this grant will help improve the process
In hemophilia A, which accounts for about 80% of all cases, patients do not produce enough of a clotting protein called factor VIII (FVIII). To better understand the mechanisms that are mitigating the effects of current drug candidates, Herzog is teaming up with some of the nation’s leading experts.
Their program will focus on three major projects in gene therapy for hemophilia A:
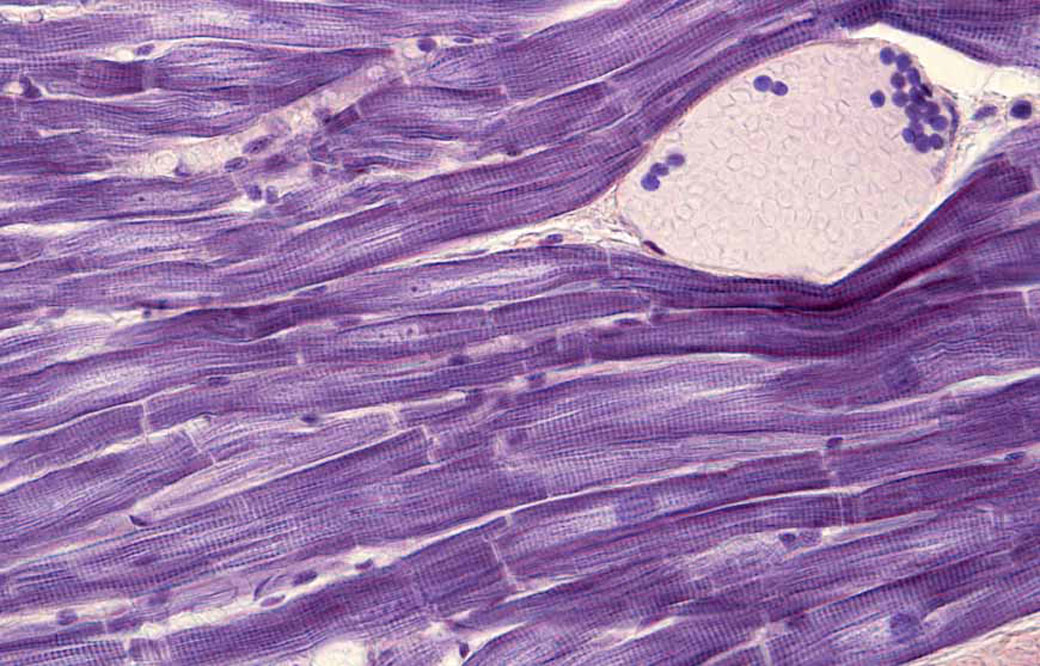
- Project 1 will focus on cellular toxicity and stress that can be induced by FVIII protein production. This project is led by Kaufman.
- Project 2 will focus on molecular virology and the development of viral vectors used in gene therapy to deliver the FVIII-encoding gene.This project is led by Indiana University School of Medicine professor of pediatrics Weidong Xiao, PhD
- Project 3 will examine the immune system and its role in the interference of FVIII production over time. It is jointly led by Herzog and Ype P. de Jong, MD, PhD, assistant professor of medicine at Cornell University.
Together, they hope to provide new insight that can lead to lower levels of toxicity and improved longevity of FVIII production in patients who are treated with gene therapy for hemophilia.
“This is an incredibly significant and urgent medical question, and it requires the synergy of multiple groups with different expertise to come together and solve a problem that they wouldn’t be able to solve on their own,” says Herzog. “My hope is that our studies will help the field as a whole move toward curing hemophilia A.”
The grant is titled “Toward Safer Gene Therapy for Hemophilia A” (P01HL160472). This post was adapted from a press release published by Indiana University School of Medicine.