Infectious disease expert Sumit Chanda tells us how his team is combating the virus, and the advice he gives his loved ones.
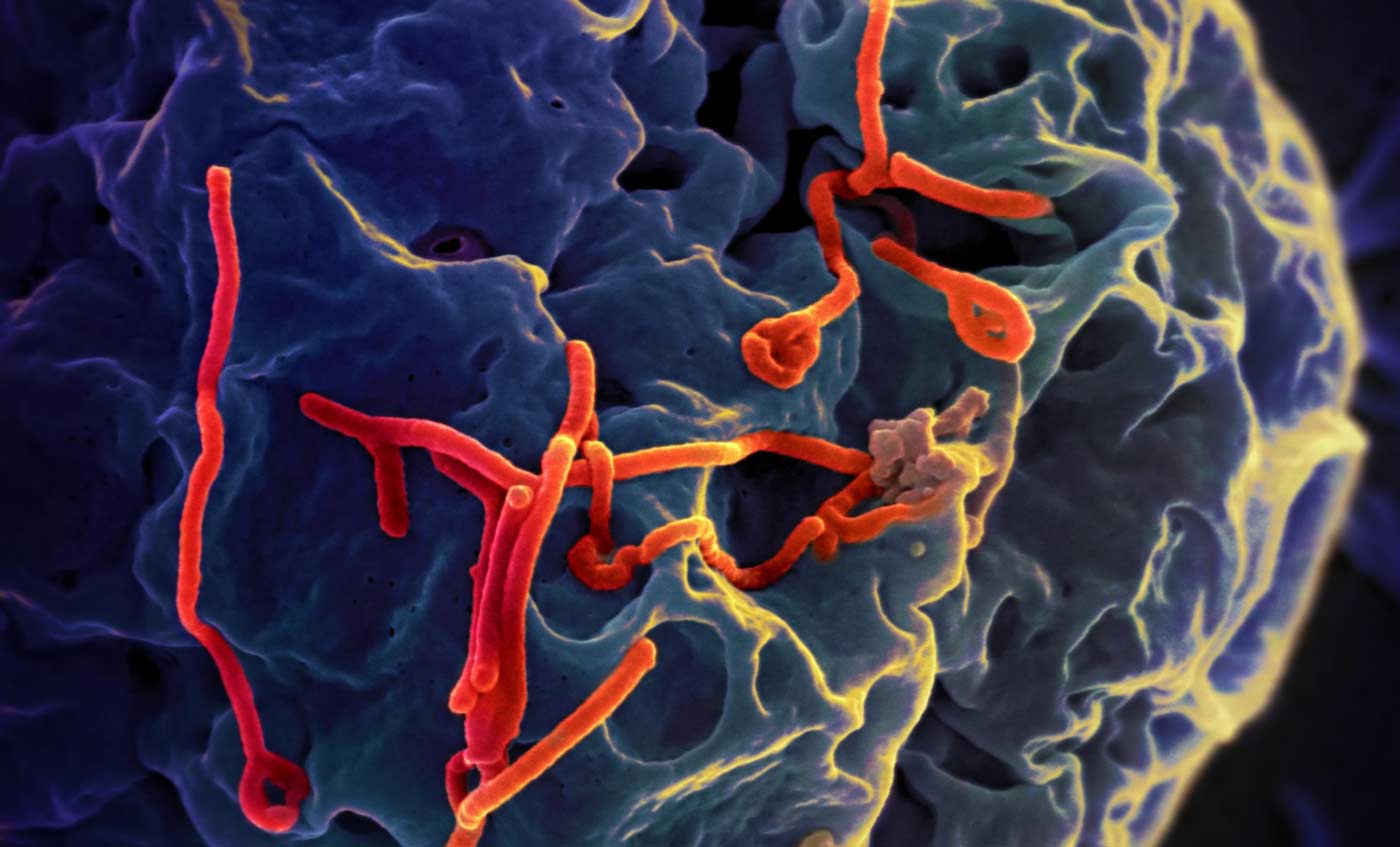
Since the first case of coronavirus (COVID-19) was identified in December 2019, the respiratory virus has swept across the globe. Cases have been confirmed on every continent but Antarctica, prompting the World Health Organization to declare COVID-19 an official pandemic.
As the world grapples with the ongoing outbreak, we spoke with Sumit Chanda, PhD, an infectious disease expert and director of Sanford Burnham Prebys’ Immunity and Pathogenesis Program, to get his perspective on the pandemic and learn what Sanford Burnham Prebys scientists are doing to find effective treatments for COVID-19.
What is coronavirus?
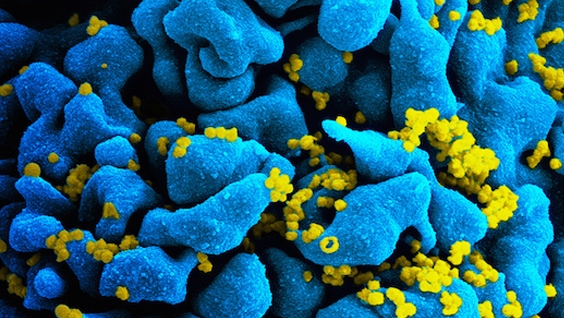
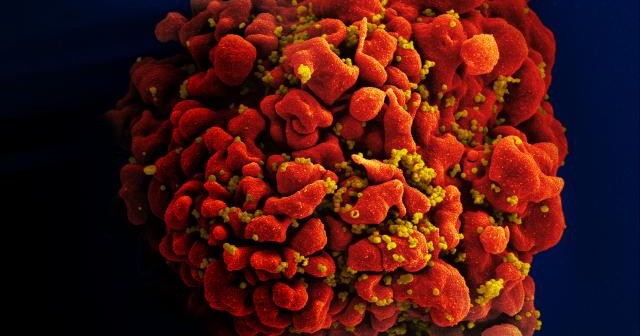
Coronaviruses are a large family of viruses common in animals, but they can leap to humans, causing illnesses ranging from a common cold to severe respiratory diseases such as pneumonia, Middle East respiratory syndrome (MERS), and severe acute respiratory syndrome (SARS).
Were you surprised by the virus’s rapid spread? Why or why not?
Once there was evidence of person-to-person transmission outside of China, the rapid global spread of the virus was not surprising. Since this is a new virus, there is no natural immunity in the human population to slow the spread of the pathogen. Furthermore, respiratory viruses are among the most easily spread microbes and thus considered to have high pandemic potential.
Is there a vaccine for COVID-19?
Since this is a new coronavirus, there is no vaccine—and developing one can take several years.
How are Sanford Burnham Prebys scientists working to combat COVID-19?
As we speak, our scientists are looking to find known drugs that can inhibit the virus. Typically, it can take five to 10 years to bring a new drug to the market. However, the approach we are taking at Sanford Burnham Prebys, known as drug repositioning, can cut this development time dramatically. Since we are looking at FDA-approved drugs that are proven to be safe in humans, these medicines could rapidly get to people infected with the virus. If successful, drug repositioning will likely be the fastest path to find a therapeutic solution for the virus.
Longer term, work has been ongoing to develop broad-spectrum antivirals. These medicines would work against many viruses, not just one. For example, if we had developed a broad-spectrum antiviral that works on MERS or SARS, it is likely it could be used for the current COVID-19 outbreak. Ideally, the therapy could be given prophylactically to block the rapid spread of the disease.
What are the benefits of drug repositioning?
Drug repositioning is advantageous because FDA-approved drugs have already completed safety testing—meaning they have been used in people and are known to be safe. Safety testing can take years to complete. This means that if we do find a therapy that is effective against COVID-19, we can bring it to patients much faster than a novel treatment.
Any predictions for how far the virus will spread in the U.S.?
We eagerly await large-scale testing for the virus so we can get a better understanding of how widespread it currently is in the U.S. It is difficult to predict a potential trajectory of viral spread in the U.S. until those numbers become available.
But as of now, I have not seen any evidence of disease containment. It will be instructive to see how the situation plays out in other advanced democracies that are coping with a viral outbreak, including South Korea and Europe, to get a better idea of what might happen here.
Get an inside look at the race to find a treatment for COVID-19.
What advice are you giving your loved ones?
The advice I give my friends and family is to hope for the best, prepare for the worst. We are in uncharted waters.