Evan Snyder tells us how he is using lung organoids to find effective treatments for COVID-19.
As the novel coronavirus races around the globe, mystifying patterns are emerging. The virus seems to hit some people hard—including men, people over the age of 65 and individuals with pre-existing medical conditions. For others, particularly children, the symptoms may be mild or even nonexistent.
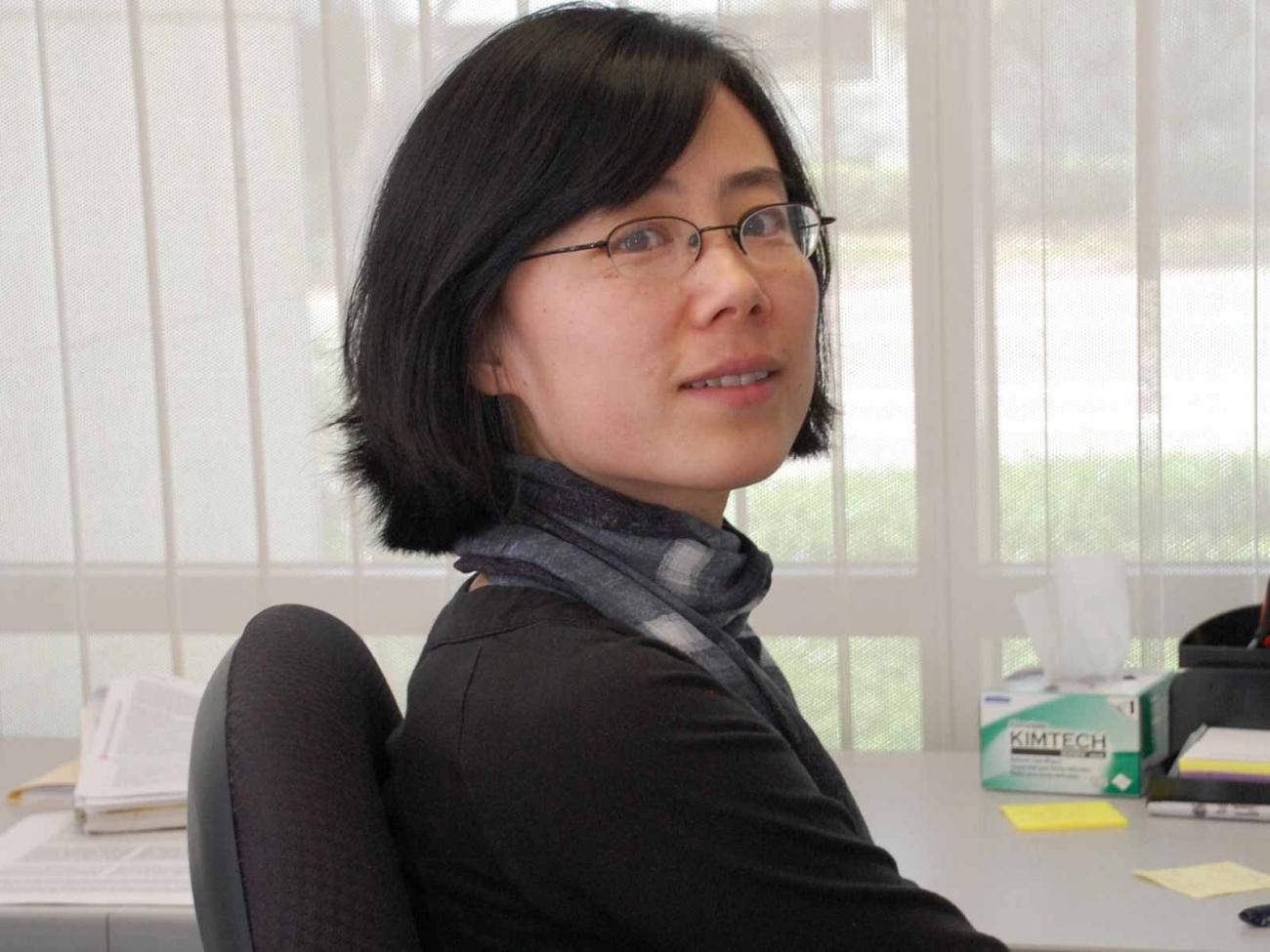
To understand why these disparities occur, stem cell expert Evan Snyder, MD, PhD, director of Sanford Burnham Prebys’ Center for Stem Cells and Regenerative Medicine, is turning to lung organoids—3D structures that replicate human lungs.
We caught up with Snyder to learn more about these “mini lungs” in a dish—and how the outbreak has impacted his lab.
Why did you create these organoids?
A neonatologist who works in my lab, Sandra Leibel, MD, originally developed these organoids to see if we could help babies who have trouble breathing. Premature babies, and some full-term babies born with genetic conditions, can’t make surfactant—the material that allows the lungs to be flexible and breathe. The severe respiratory distress that is thought to kill some people with severe COVID-19 is actually the adult version of what these babies experience.
I’m happy to report that, using this model, Sandra was able to find a therapy that might help these infants with the previously untreatable genetic condition. I’m hoping we can learn from this success to help people with severe COVID-19 and “adult respiratory distress syndrome.”
How are these lung organoids made?
We start with human induced pluripotent cells (hiPSC) created from skin cells and turn these into lung cells using the same chemical signals our body uses. Then the exciting part comes: We transform these cells from flat, two-dimensional layers into three-dimensional spheres that grow the way a lung would—aka “mini lungs in a dish.” Sandra, along with technician Alicia Winquist and Sanford Burnham Prebys graduate student Rachael McVicar, figured out the “secret sauce” the cells need to complete this process.
What makes these lung organoids so special?
Lungs are very complicated organs. They have many cell types and structures that all interact with each other: air sac cells that make surfactant, airway cells, immune cells, blood vessel cells; and cells with cilia, tail-like organelles that whip around and clear out debris. Our organoids contain all these different parts, so they can be used to model human disease more closely than single layers of cells. They’re also easier to scrutinize, manipulate and test treatments in animal models. These organoids let us ask and answer all sorts of interesting questions.
What do you hope to learn about COVID-19 using this model?
We want to learn the basics about the virus that causes COVID-19, called SARS-CoV-2. For example, how does the virus infect human lung cells? What does the virus do after it enters the lung cell? How does the virus move from one lung cell to another? The answers to these questions will allow us to find effective treatments for COVID-19.
In addition, we can use this model to determine why some people fare worse than others. We can compare organoids created from men and women; younger or older people; people exposed to various environmental toxins from smoking or vaping; people with diabetes, heart or kidney disease; and even people of different racial backgrounds or individuals who have genetic variations that affect their ability to fight infection.
If we figure out why the virus affects some people differently, we can potentially create tailored treatments. For example, we can ask whether any disparities we observe can be compensated for simply by increasing a dose of a drug or by adding another drug. With our model, we may be able to find these answers relatively quickly so that as many people as possible can benefit from any breakthroughs.
Will you partner with additional Sanford Burnham Prebys scientists on this research?
Yes, we are in a fortunate position to collaborate with Sumit Chanda, PhD, who just completed a heroic (and I do mean heroic) effort to screen 12,000 known drugs for COVID-19. He pinpointed 30 promising drugs, and now we will help him study exactly how these drugs are working in a system that is clinically relevant. For example, in what stage of the virus’s life are they disrupting? Which part of the cell’s function is being rescued? Using lung organoids, we can rank the effectiveness of each drug—and help Sumit winnow the list to the most promising drugs for close-to-immediate use.
The best approach to treat COVID-19 will most likely be with a drug cocktail, similar to how we treat other RNA viruses. For this reason, it’s important to know how each drug is working, because we want to attack the virus at multiple points in its life cycle and block toxic downstream effects. Our model will help us map this out and advance the most promising drug combinations.
How has the outbreak affected your lab work?
I have time-sensitive, patient-relevant work ongoing, so I am still coming into the lab. In addition to our COVID-19 work, we are preparing to launch a clinical trial using stem cells to help newborns who are at risk for cerebral palsy.
However, things are very different now. When I do go in, there are only one or two people instead of dozens, and we work in shifts. We limit our time to a few hours and only come in a few days a week. What I really miss is the meeting of the minds. Some of the most inspirational science comes from sitting around in a group and sharing ideas. Or having someone walk over and look through your microscope at the primary data. We do our best with Zoom. But the in-person human interactions are the part of science I really miss.