New study shows that targeting an oft-drugged family of cell membrane receptors with biased modulators can expand potential drug targets and reduce side effects
About one-third of all drugs approved by the Food and Drug Administration target the largest family of cell membrane receptors called G protein-coupled receptors (GPCRs).
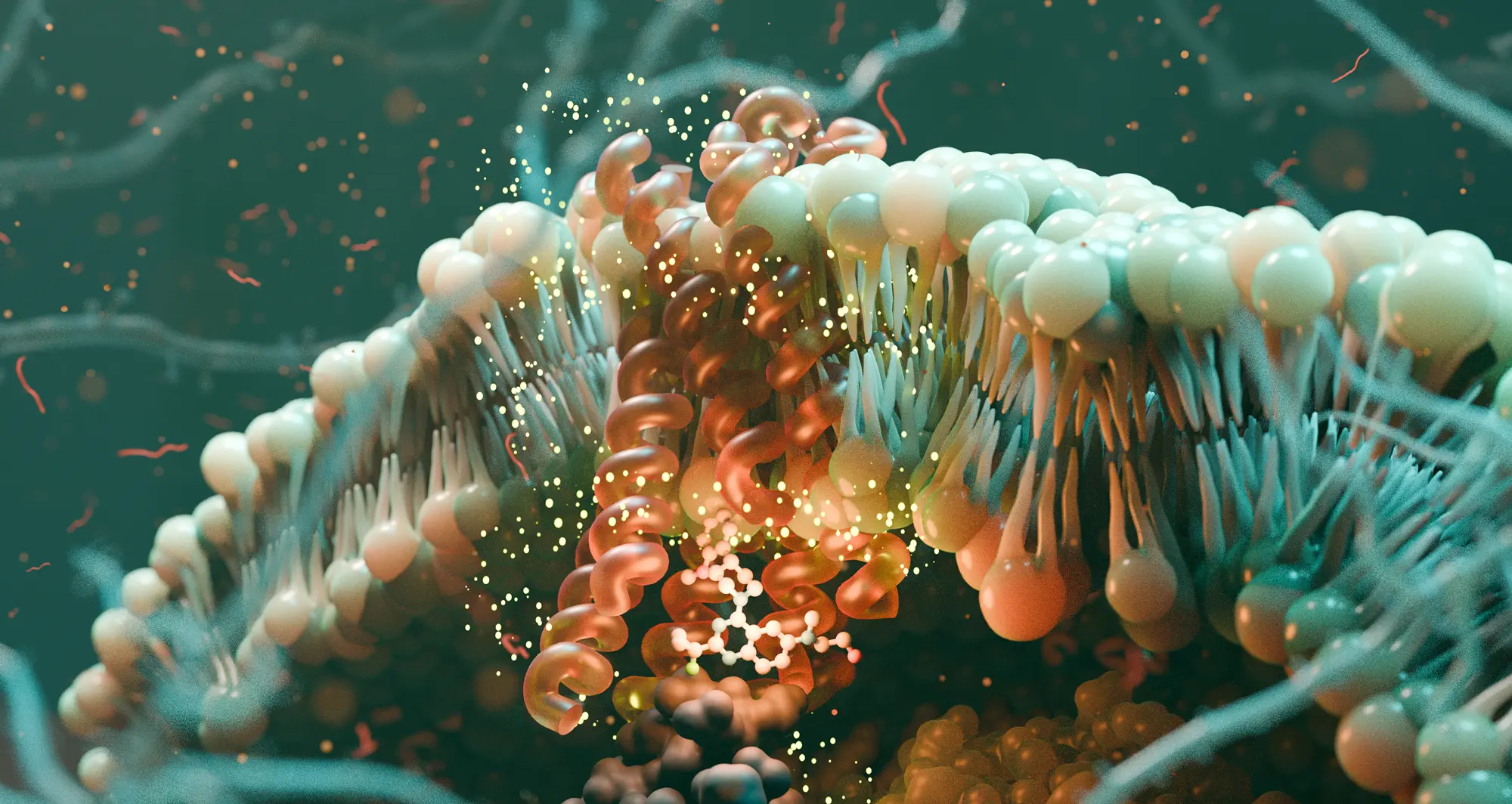
GPCRs are indispensable for maintaining human health as they play a role in nearly every physiological function. These receptors are embedded in the membranes of cells and detect a wide variety of biological signaling molecules arriving outside the cell. These signals then activate proteins called G proteins and beta-arrestins inside the cell to carry out the many jobs governed by this family of receptors.
As plentiful as GPCR-based drugs are, scientists recognize that these receptors still hold untapped potential as targets for new treatments.
“Out of 826 GPCRs, approximately 165 are validated drug targets so many of them have not been drugged,” said Steven Olson, PhD, the executive director of Medicinal Chemistry at the Sanford Burnham Prebys Medical Discovery Institute’s Center for Therapeutics Discovery.
“Some of this gap is because the binding pocket on the extracellular side can be too small, too large or no obvious binding site can be found. Our work takes advantage of the fact that the intracellular side always binds G proteins or beta-arrestin, so there’s nearly always going to be a binding pocket there.”
Scientists at Sanford Burnham Prebys, the University of Minnesota and Duke University published findings October 22, 2025, in Nature demonstrating how a small molecule can bind a GPCR on the inside of the cell and bias or more specifically direct the receptor’s signaling. If drug designers can control how compounds bias signaling, they can leverage those that favor therapeutic pathways while preventing changes in other pathways that result in unwanted side effects.
All but four of the FDA-approved drugs targeting GPCRs bind the side of their intended receptors that sits outside the cell and relatively few demonstrate pronounced signaling bias.

Steven Olson, PhD
Image credit: Sanford Burnham Prebys.
“People have understood the need for bias in drug design for a long time,” said Lauren Slosky, PhD, an assistant professor of Pharmacology at the University of Minnesota, and the corresponding author of the study.
“These compounds, however, have been especially challenging to create because our understanding of how signaling bias is achieved is incomplete. Here we discovered a new mechanism by which intracellular small molecules can confer signaling bias in predictable ways, permitting rational design. The structure-to-activity relationships are incredibly complex, however, and the tools to unravel them have only been developed in the last few years.”
The research team first sought to better understand binding to a GPCR called neurotensin receptor 1 (NTSR1) by a biased small molecule called SBI-553. They also investigated the sixteen G proteins and two beta-arrestin proteins that can be activated by receptor signaling.
“We quickly started to appreciate that the black-and-white view we’d had, which was that our compound turned the G proteins off and the beta-arrestin on, was way too simple,” said Slosky. Rather than all-or-nothing adjustments, the investigators found that SBI-553 generated a wide range of activity levels in different G proteins and beta-arrestins.
Understanding what causes a compound to be a biased modulator is a key step in enabling the design of compounds with more precision in the array of G proteins that they activate. The scientists demonstrated that SBI-553 biases NTSR1 signaling by acting as a molecular bumper for some of the G proteins and as molecular glue for others.
“When bound, SBI-553 serves as a molecular bumper blocking the typical way G proteins bind with NTSR1,” said Olson, an author of the manuscript. “It can also act as a molecular glue promoting the binding of certain subtypes of G protein that can achieve an alternative binding conformation.”
The scientists hypothesized that modifying SBI-553 could change the way it biased signaling to favor different G proteins and beta-arrestins. They tested a panel of 29 compounds similar to SBI-553 that contained small structural adjustments. These drugs varied significantly in their activation and inhibition of the G protein subtypes and beta-arrestins.
“We showed that small differences in the molecule can lead to big differences in the downstream signal,” said Slosky.
“And that you can change which ones get turned on and which ones get turned off based on targeted changes in the chemical structure of the modulator,” said Olson. “Most importantly, these changes are predictable and can be used by medicinal chemists to rationally design new drugs.”
Researchers have explored targeting NTSR1 to treat addiction and other psychiatric disorders for decades, but drug discovery efforts have been stymied by severe side effects. Unlike unbiased compounds that did not prove safe in targeting this receptor, the scientists showed in prior research that SBI-553 avoids problematic side effects, which include hypothermia and hypotension.
The research team theorized that activation of a particular G protein was at fault for these side effects. Because SBI-553 fully inhibits Gq, the suspected problem protein, they tested this theory by comparing the effects of the compound to a similar small molecule called SBI-593 incapable of fully blocking Gq.
“Unlike SBI-553, in mice treated with a balanced agonist, SBI-593 was unable to prevent hypothermia,” said Slosky. “In this case, a small change in the structure led to changes in signaling and biology.”
In the wide world of GPCRs including NTSR1, this new drug discovery approach opens up many more receptors previously considered “undruggable” as potential drug targets.
There have been few biased drugs for GPCRs developed in the past because the interactions are so complex that they haven’t been predictable. By discovering molecules that bind to the intracellular site, the molecular mechanisms responsible for bias are far more predictable because the molecules directly interact with both the GPCR and the G proteins, acting as bumpers or glues.
“We’ve now shown that this intracellular site is druggable, and it opens up an enormous field of study,” said Olson. “Moreover, we also demonstrated that the interactions are predictable, which is an important factor for anyone investing in drug discovery.”
Madelyn Moore, a graduate student in the Slosky lab at the University of Minnesota, shares first authorship of the study with Kelsey Person, also a graduate student in the Slosky lab.
Additional authors include:
- Michael R. Jackson from Sanford Burnham Prebys
- Abigail Alwin, Campbell Krusemark, Noah Foster, Michael J. Sheedlo and Ezequiel Marron Fernandez de Velasco from the University of Minnesota
- Caroline Ray and Lawrence S. Barak from Duke University
- Asuka Inoue from Tohoku University and Kyoto University
The study was supported by the National Institutes of Health, National Institute on Drug Abuse, Department of Defense, University of Minnesota Foundation, Japan Society for the Promotion of Science, Japan Agency for Medical Research and Development and Japan Science and Technology Agency.
The study’s DOI is 10.1038/s41586-025-09643-2.
The bottom line on biased modulators
What problem is this research trying to solve?
Roughly one-third of all FDA-approved drugs target the largest family of cell membrane receptors called G protein-coupled receptors (GPCRs). The first problem we’re addressing is that there is still a lot of untapped potential in this field. Many GPCRs have not been successfully targeted because of challenges with getting drugs to bind the receptors, or due to side effects that occur.
The second problem is that the drugs targeting GPCRs are unbiased modulators. Because these dramatically change the signaling system, you can generate beneficial effects while also creating unintended side effects. If we can control how compounds bias signaling, then we can leverage those that favor therapeutic pathways while preventing changes in other pathways that result in unwanted side effects.
What did you find in this study?
First, we have demonstrated how a small molecule can bind a GPCR on the interior side of the cell. All other GPCR-based drugs target the exterior side. Having the ability to target the interior side may open up many “undruggable” GPCRs as targets for future medications.
One thing that is novel here is the ability to design drugs that bind in this intracellular pocket. No one has tried to do this. The other novel thing is that while some biased compounds can differentiate between the two major signaling pathways, it’s rare or perhaps even unprecedented to differentiate within one of those pathways. In the G protein pathways, there are 14 different G proteins, and we can differentially activate and deactivate those.
In addition, we have shown how modern drug discovery tools enable the creation and optimization of a new class of drugs that are biased modulators binding to the intracellular pocket of GPCRs. This is important because this is the pocket where the signaling proteins bind, so it gives opportunities for unprecedented control in the signaling process. We describe in the paper that these compounds are bumpers or glues for different G proteins.
Institute news on biased modulators
Sanford Burnham Prebys announced in October 2019 the receipt of a $3.58 million NIH grant to advance research on SBI-553 as a potential treatment for opioid-use disorders.
The grant was awarded as part of the Helping to End Addiction Long-term Initiative, or the NIH Heal Initiative, which awarded a total of $945 million in fiscal year 2019 to accelerate scientific solutions to address the national opioid crisis.
In November 2023, the institute announced that the collaborators working on this project had recently received a $6.3 million award from NIH and the National Institute on Drug Abuse to advance their addiction drug candidate, called SBI-810, to the clinic.
SBI-810 is an improved version of SBI-553. This funding is being used to complete preclinical studies and initiate a Phase 1 clinical trial to evaluate safety in humans.
SBI-553: a scholarly timeline
In 2019, the team reported the discovery of SBI-553 in the Journal of Medicinal Chemistry.
In Cell in 2020, the scientists detailed SBI-553 as a biased modulator that reduces stimulant effects without the side effects of unbiased NTSR1 agonists.
In 2023, the researchers published a structural analysis of the binding site and structural determinants for biased modulation by SBI-553 in Biochemistry.
In Addiction Neuroscience in 2024, the group demonstrated SBI-553’s potential for treating alcohol use disorders by showing that it reduces ethanol drinking and responses to ethanol administration in rodents. Zoe McElligott, PhD, associate professor of Psychiatry and Pharmacology at the University of North Carolina School of Medicine, was the corresponding author of the study.
In August 2025, the scientists described in Cell the effects of an SBI-553 analog called SBI-810, highlighting NTSR1-biased allosteric modulators as a promising, non-addictive therapeutic strategy for acute and chronic pain management. Ru-Rong Ji, PhD, William Maixner Professor of Anesthesiology at Duke University School of Medicine, was the corresponding author of the study.