Sanford Burnham Prebys professor José Luis Millán, PhD, has joined a five-year, $13 million program that will study misplaced calcification in the eyes and brains of patients suffering from age-related macular degeneration (AMD) and Alzheimer’s disease (AD).
The initiative is funded by the National Institute on Aging and will be led by Francesca Marassi, PhD, an adjunct professor at Sanford Burnham Prebys and chair of biophysics at the Medical College of Wisconsin.
AMD affects nearly 20 million adults in the U.S. and is the leading cause of central vision loss and legal blindness. AD affects more than 6 million people in the U.S., and it is the top cause of dementia across the globe. Age is a prominent risk factor for both diseases. However, how AMD and AD progress over time is not well understood, and research is needed to drive the development of effective pharmaceutical treatments.
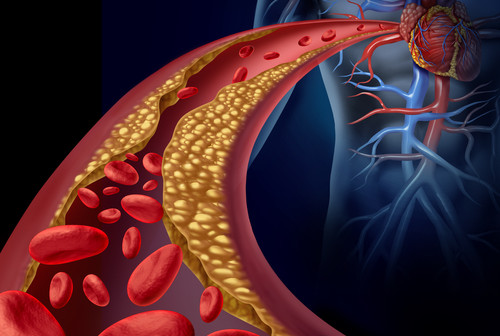
Both diseases are associated with the progressive accumulation of mineralized deposits under the retina and in the brain. Healthy calcification processes are needed to grow and repair bones, but these same processes can cause misplaced deposits in the eye and the brain that contribute to disease. Scientists do not yet know what causes these deposits to form, and answering this question may provide clues to better understand AMD and AD, as well as aid the development of new ways to diagnose and treat these diseases.
The international research team, which also includes scientists from UC San Diego, University of Maryland School of Medicine, and Queen’s University Belfast, will explore the characteristics of misplaced calcifications in both the eye and the brain. They have devised four projects to examine calcifications at varying scales, from their atomic structure up to their accumulation in cells and animals.
Millan will direct the fourth project, which will study how cells and tissues maintain their balance of phosphorus. In human adults, approximately 90 percent of the body’s total phosphorus is crystalized in bone, and these same crystals also are part of the calcified deposits that form in AMD and AD. Dr. Millan’s team will study mice to determine how cells control phosphorus levels and how these biochemical pathways contribute to the formation of calcified deposits in the eye.
The grant, funded by the National Institute on Aging, is titled “Molecular mechanisms of calcification: roles and opportunities in diseases of aging.”
This story is adapted from a press release published by Medical College of Wisconsin.