Carbapenems are a class of highly effective antibiotics that are often used to treat severe bacterial infections. They are usually reserved for known or suspected bacterial infections resistant to other drugs.
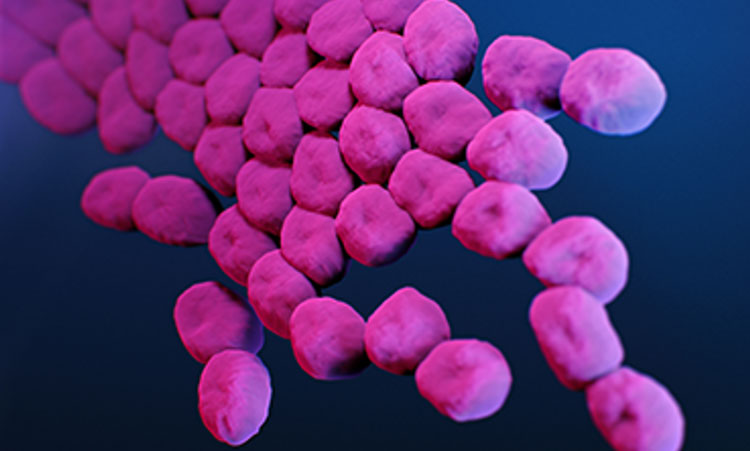
Carbapenem-resistant Acinetobacter baumannii (CRAB) is, as the name suggests, impervious to carbapenems; and it has become a major global pathogen, particularly in hospital settings and conflict zones. No new antibiotic chemical class with activity against A. baumannii has successfully emerged in more than 50 years.
In a paper published January 3, 2024, in Nature, a multi-institutional team including Andrei Osterman, PhD, at Sanford Burnham Prebys, with colleagues at Roche—the Swiss-based pharmaceutical/healthcare company—and others, describe a novel class of small-molecule tethered macrocyclic peptide (MCP) antibiotics with potent antibacterial activity against CRAB. Osterman’s lab provided critical data and discoveries related to the drug target and mapping of drug-resistant mutations.
Developing a new class of antibiotics effective against CRAB is critical. The bacterium is resistant to nearly all antibiotics and is difficult to remove from the environment. It poses a particular health threat to hospitalized patients and nursing home residents, with an estimated mortality rate in invasive cases of 40–60%.
The World Health Organization and the Centers for Disease Control (CDC) have both categorized multidrug-resistant A. baumannii as a top-priority pathogen and public health threat.
In the new study, Osterman and colleagues applied an experimental evolution approach to help identify the drug target (the LPS transporter complex) of a new class of antibiotics—a macrocyclic peptide called Zosurabalpin—and elucidate the dynamics and mechanisms of acquired drug resistance in four distinct strains of A. baumannii.
They used an integrative workflow that employs continuous bacterial culturing in an “evolution machine” (morbidostat) followed by time-resolved, whole-genome sequencing and bioinformatics analysis to map resistance-inducing mutations.
In addition to a mechanistic understanding (crucial from a regulatory perspective), the new information also helped reveal the drug-binding site. A related paper in the same issue experimentally verified the findings.
“This comprehensive mapping of the drug-resistance landscape yields valuable insights for a variety of practical applications,” says Osterman, “from therapy optimization via genomics-based assessment of drug resistance/susceptibility of bacterial pathogens to a rational development of novel drugs with minimized resistibility potential.”
A commentary in Nature said the research was “cause for cautious celebration” and urged further development.