Sanford Burnham Prebys scientist works on new methods to boost the body’s natural defenses against melanoma and other cancers
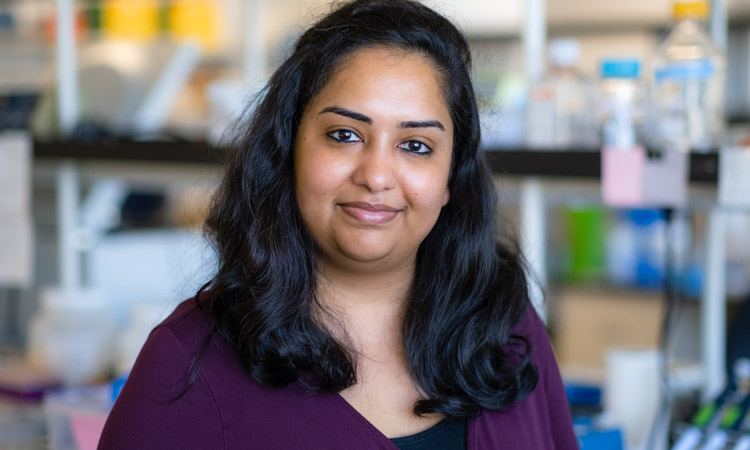
When she was growing up in India, Sreeja Roy, PhD, looked up to her father as he applied his scientific knowledge to care for the patients in his medical practice.
“He was my inspiration,” says Roy. “I found that I was particularly good at biology, and I liked learning about the mechanisms of how things work. Along the way, I realized I didn’t want to be a medical doctor and began focusing on biomedical research—and I fell in love with it.”
After earning her undergraduate degree in biotechnology from The Australian National University in Canberra, Roy obtained a master’s degree in infection biology from the Universität zu Lübeck in Germany. She returned to The Australian National University for her doctoral degree in immunology with an emphasis on viral vector-based vaccine immunology. After completing graduate school, Roy worked as a postdoctoral researcher at Albany Medical Center in New York before joining Sanford Burnham Prebys in September 2021 as a postdoctoral associate in the Immunity and Pathogenesis Program.
“I had been working on basic science in Albany,” notes Roy. “I really wanted to do translational research so I could work on things that would benefit people much sooner. That is why I chose to move to Sanford Burnham Prebys and focus on cancer immunotherapy.”
Roy’s background in immunology prepared her to enter the emerging field of cancer immunotherapy. This discipline involves developing treatments that enhance the human body’s innate immune response to better locate and dispose of cancer cells. She learned about an opportunity to support her interest in translational immunotherapy through the Jean Perkins Foundation Fellowship.
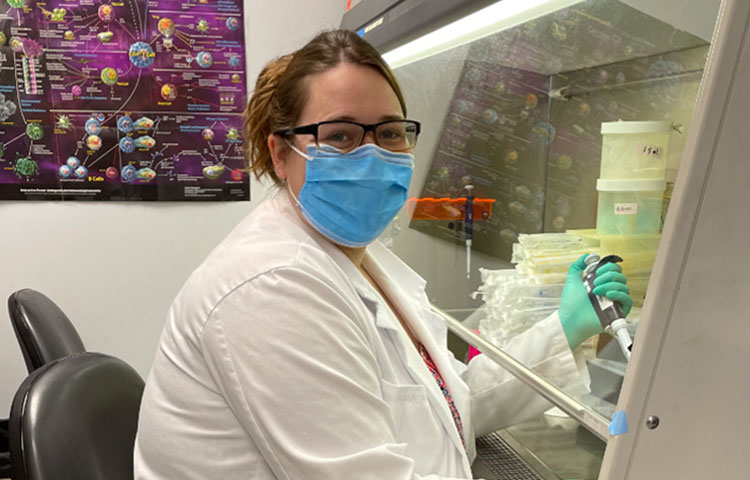
Roy received one of two prestigious fellowships designed to support postdoctoral researchers in the lab of Carl Ware, PhD, director of the Infectious and Inflammatory Diseases Center and professor in the Immunity and Pathogenesis Program.
“The Jean Perkins Foundation Fellowship has been fantastic,” says Roy. “I can work without the pressure of writing an academic grant, which allows me to focus on the science and be more productive.”
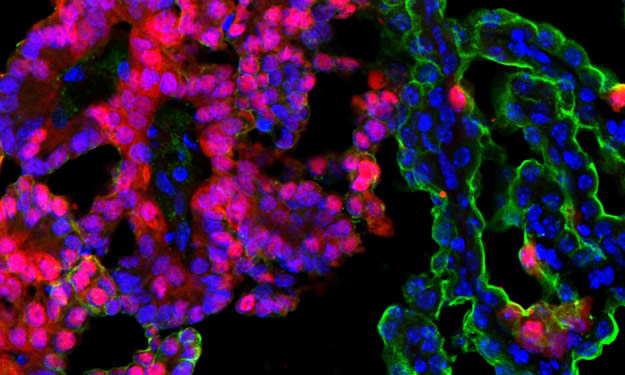
Roy’s project at the Ware lab involves making immunotherapies more effective in treating melanoma, the deadliest form of skin cancer.
“Unfortunately, some tumors never respond to immunotherapy treatments,” explains Roy. “Also, tumors can initially begin to shrink before becoming resistant to a treatment.”
Under Ware’s direction, Roy is testing ways to enhance existing immunotherapies through the lymphotoxin-β receptor, which is found on some types of immune cells.
“When the immune system encounters a foreign substance that may cause an infection, a sample of the invader can be shuttled to the lymph nodes as a way of learning about the threat and generating a better immune response,” explains Roy. “Depending on which tissues are being infected, the lymph nodes cannot always be involved, so an active lymphotoxin-β receptor is able to approximate their effect by organizing immune cells in something akin to training centers so that a better attack can be launched.”
Roy and the Ware lab are developing ways to take advantage of the lymphotoxin-β receptor’s ability to recruit and train immune cells as an approach to making immunotherapies more effective.
“If I can target the lymphotoxin-β receptor signaling against tumors, does that enhance the anti-tumor immunity?” asks Roy. “Do the tumors become more responsive to the treatments now? That is what we’re trying to find out.”
With the help of the Jean Perkins Foundation Fellowship, Roy is determined to continue developing her translational science expertise and find ways to improve the effectiveness of immunotherapies for melanoma and other cancers.
“We’ve made quite a bit of progress,” says Roy. “I look forward to sharing our results and seeing how this project advances from the bench to the bedside.”