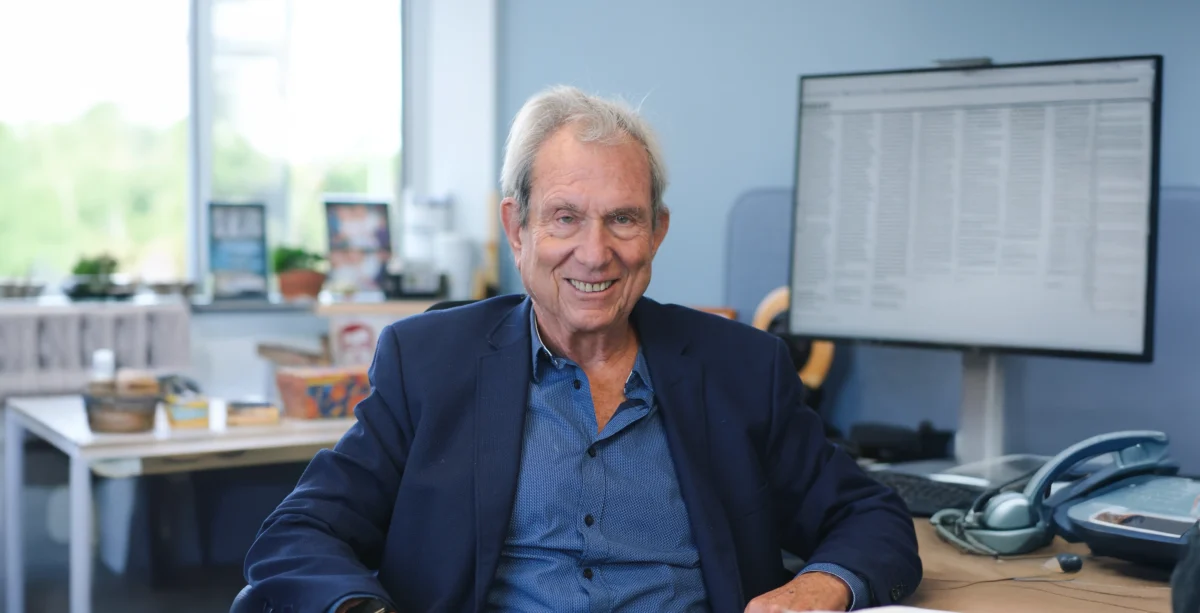
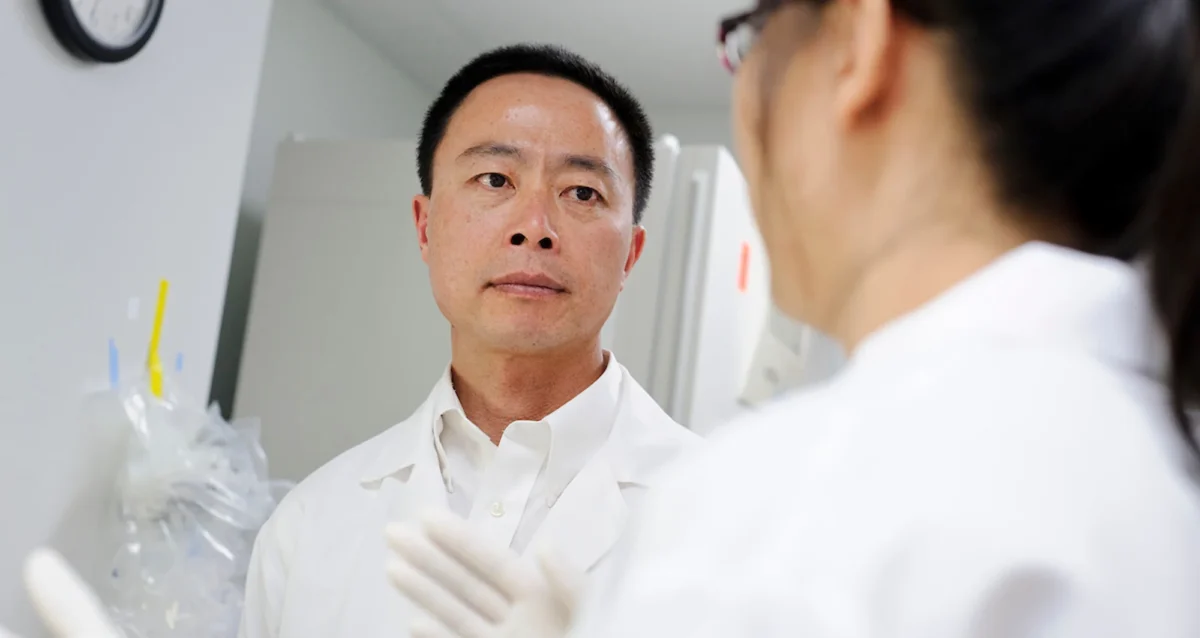
Dr. Boutros was trained in Chemistry at the University of Waterloo (BSc, 2004) and Medical Biophysics at the University of Toronto (PhD, 2008). He then began his independent research career at the newly-formed Ontario Institute for Cancer Research, where he
remained until 2018. That year, he relocated to UCLA, where he served as the inaugural Director of Cancer Data Science, Interim Vice-Dean for Research, and was appointed as a full professor in the departments of Human Genetics & Urology.
Dr. Boutros is renowned for his work on integrating computational and data science into cancer research. He has worked extensively with artificial intelligence and machine learning to identify new cancer biology, new drug targets and new biomarkers. Linked
to these discoveries have been major new datasets and software that serve as resources to accelerate global research in oncology, and beyond.
Dr. Boutros has published over 400 peer-reviewed research papers, and has received awards for his mentorship at the undergraduate, graduate and post-graduate levels. In 2018 he was recognized with the prestigious Dorval Prize by the Canadian Cancer Society.
Education
2016: MBA, Rotman School of Management, University of Toronto
2008: PhD, Medical Biophysics, University of Toronto
2004: BSc, Chemistry, University of Waterloo
Honors and Recognition
2023: Excellence in Postdoctoral Mentoring Award, UCLA
2023: Outstanding BIG Research Mentorship Award, UCL
2018: Bernard and Francine Dorval Prize, Canadian Cancer Society
2016: Excellence in Graduate Mentorship Award, University of Toronto
Related Disease
Head And Neck Cancer, Prostate Cancer, Sarcoma, Thyroid Cancer
Techniques and Technologies
Computational Biology, Genomics, Machine Learning, Proteomics
Out of every five Americans, two will be diagnosed with cancer during their lifetimes. Over two million people receive a new cancer diagnosis each and every year. These millions of cancers all share many common features, like changes in their DNA and an ability to rapidly grow. But each and every cancer is also different because it develops in a unique human being, with their own distinct genetics, lifestyle and behaviour.
Dr. Boutros’ research focuses on understanding the features that lead cancer to develop in different ways, using computational techniques to mine unexpected insights from very large datasets. By understanding the development of cancer, his team identifies new ways to prevent, diagnose early and effectively treat the disease.
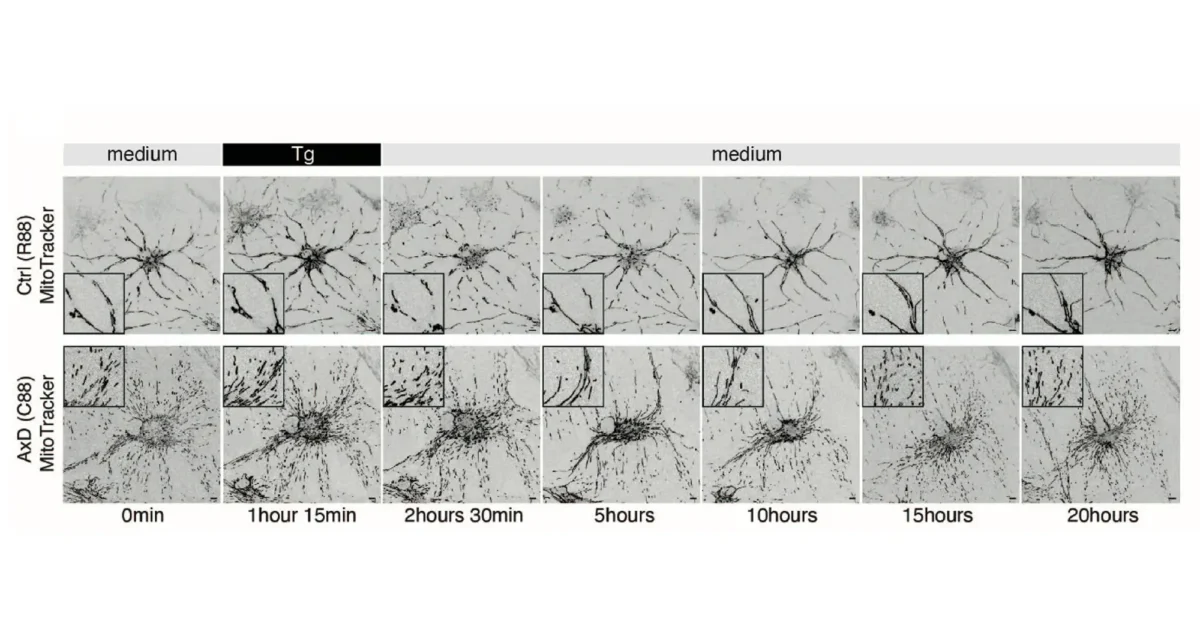
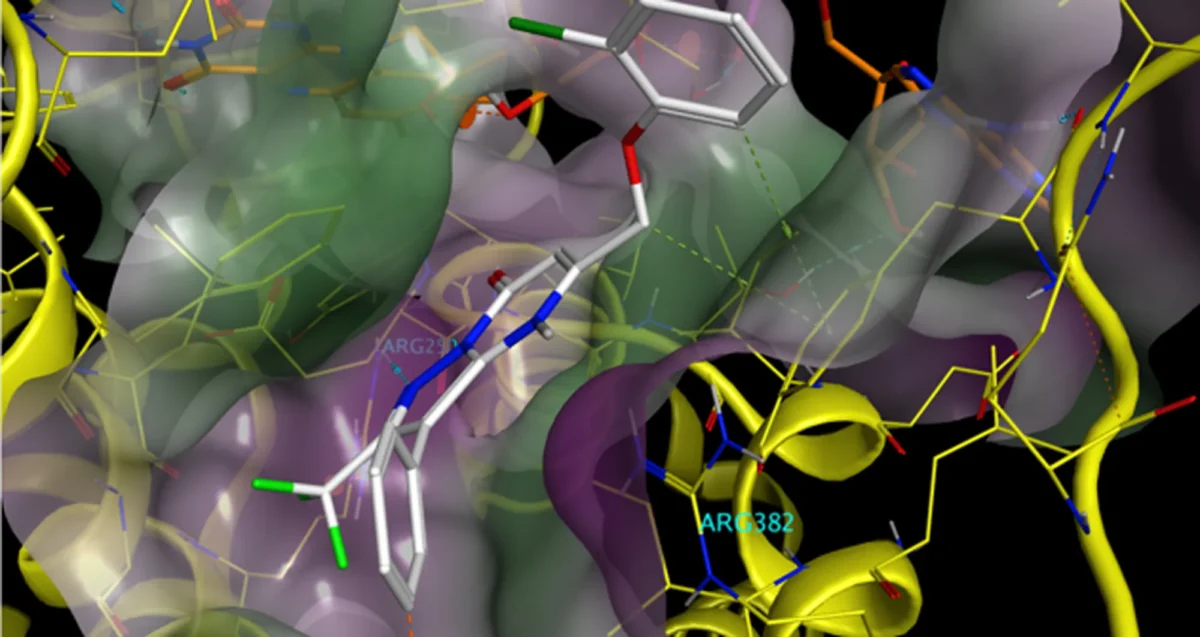
This often involves identifying generating very large new datasets by analyzing the DNA and protein content of cancers, and then creating new algorithms and AI/ML methods to analyze these data. For example, in recent work his team created a method to analyze the “dark proteome” – proteins that have been undetectable to standard analysis methods. They are now applying that method in phase 1 and phase 2 clinical trials of exercise, studying how targeted exercise therapy impacts the progression of cancer, and seeking to understand how and why exercise can be so beneficial.
 Oct 6, 2025
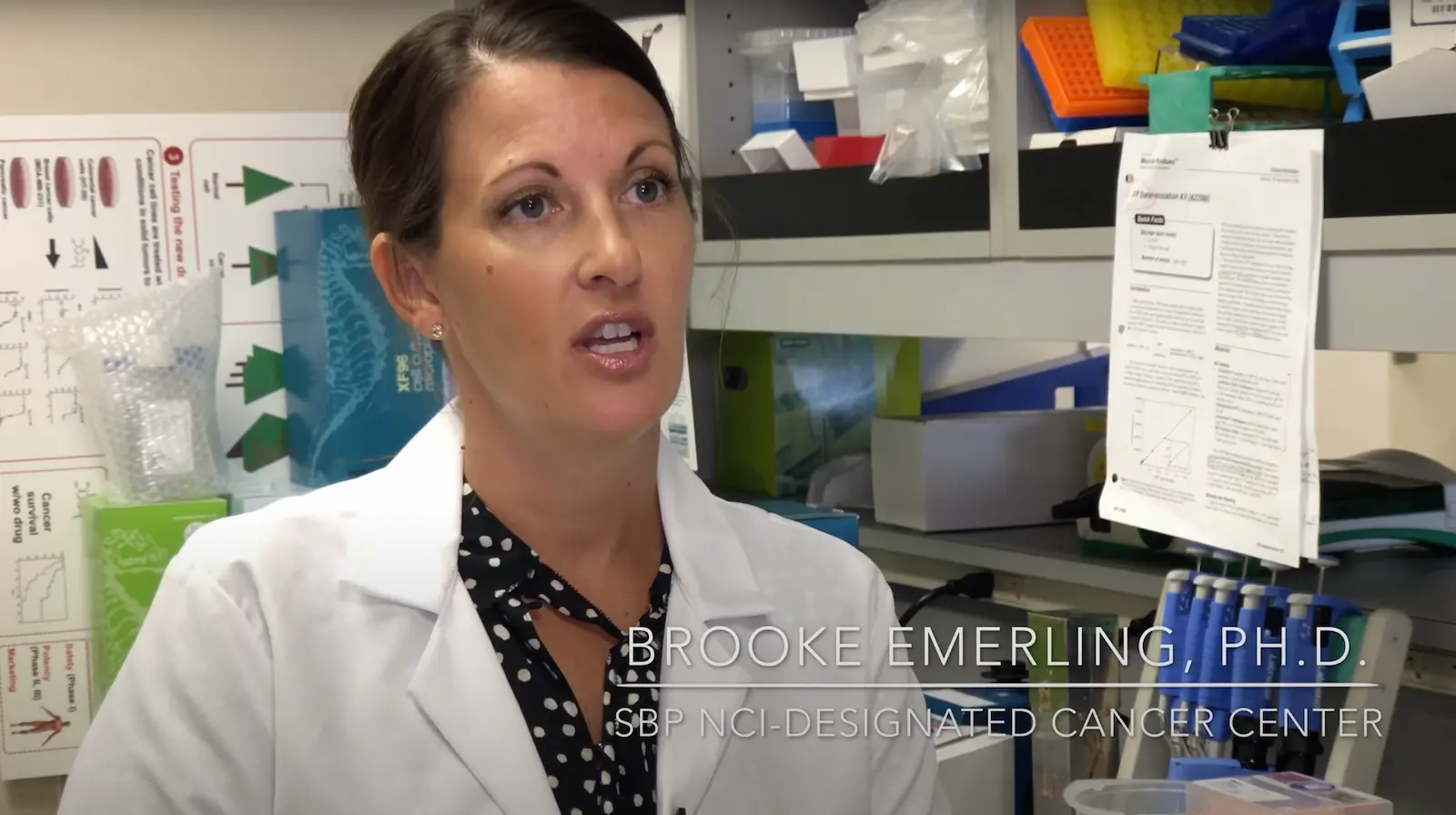
Oct 6, 2025Paul Boutros Named Cancer Center Director at Sanford Burnham Prebys
Oct 6, 2025Renowned data scientist Paul Boutros, PhD, MBA, has been named the new director of the National Cancer Institute-designated cancer center…