Child malnutrition remains an alarming and appalling scourge.
In 2022, according to the World Health Organization, 148 million children in the world under 5 years were too short for their age (stunting) and another 45 million were too thin for their height (wasting) due to inadequate diet and nutrition.
Researchers around the world, including Andrei L. Osterman, PhD, professor in the Immunity and Pathogenesis Program at Sanford Burnham Prebys, have been investigating potential remedies, in particular some of the consequences of malnutrition, such as disturbed metabolism and immune/gut function.
In a new paper published October 2, 2024 in Science Translational Medicine, the multi-institutional team (including Osterman and colleagues at SBP) describe an interventional diet that essentially repairs the gut microbiome in children with moderate to severe acute malnutrition.
They conducted a three-month randomized controlled trial of a specialized food supplement in 12- to 18-month-old Bangladeshi children living in rural and urban slums with moderate acute malnutrition who had already been treated in hospital for severe acute malnutrition. The supplement, called microbiota-directed complementary food or MDCF-2, contains chickpea flour, peanut flour, soy flour, green banana, sugar, soybean oil and a vitamin-mineral premix, a formulation designed to promote the growth of therapeutic gut bacteria and improve the overall health and balance of the gut microbiome.
They found that MDCF-2 improved weight-for-age better than the traditional ready-to-use supplementary food (RUSF) used by relief agencies and others, which is composed of more traditional ingredients like rice, lentil, sugar, soybean oil and skimmed milk powder mixed with vitamins and minerals.
When excluding children unable to continue study participation due to severe flooding during the trial, the study authors also reported improvement of stunting at a faster rate. They tied these improvements in children’s health to Prevotella copri–associated metabolic changes.
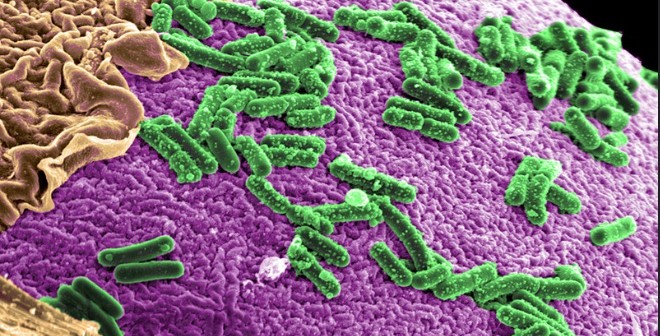
P. copri (recently renamed as Segatella copri) is a bacterium found abundantly in the human gastrointestinal microbiome. Past studies have reported both positive and negative associations with health and disease. In the former, for example, healthy bacterial colonization of the gut has been positively correlated with conditions like inflammation, insulin resistance and diarrhea. It appears to be a major player in regulating dietary metabolism.
The bacterium is more common in non-Westernized populations consuming a diet rich in plants—the bacterium’s source of nutrients. In Western populations, it is associated with consumption of fruits and vegetables.
Genomic reconstruction of the metabolic potential of P. copri strains positively associated with infants’ health improvement confirmed their unique ability to utilize a large repertoire of plant-derived polysaccharides comprising MDCF-2 diet.
“This study can be viewed as a test of the generalizability of the efficacy and mechanism of action of MDCF-2 in acutely malnourished children,” said Osterman. “The main findings include the demonstration of significantly higher efficacy of MDCF-2 vs RUSF with respect to the improvement of (weight) growth.
“The success of the treatment was also manifest by beneficial changes in microbiome composition and by global changes of a range of serum protein biomarkers associated with healthy development.”
The findings, he said, also provide proof-of-concept that improving gut microbial health can be achieved using therapeutic nutrition and offers further guidance on how best to use microbiota-directed complementary foods.