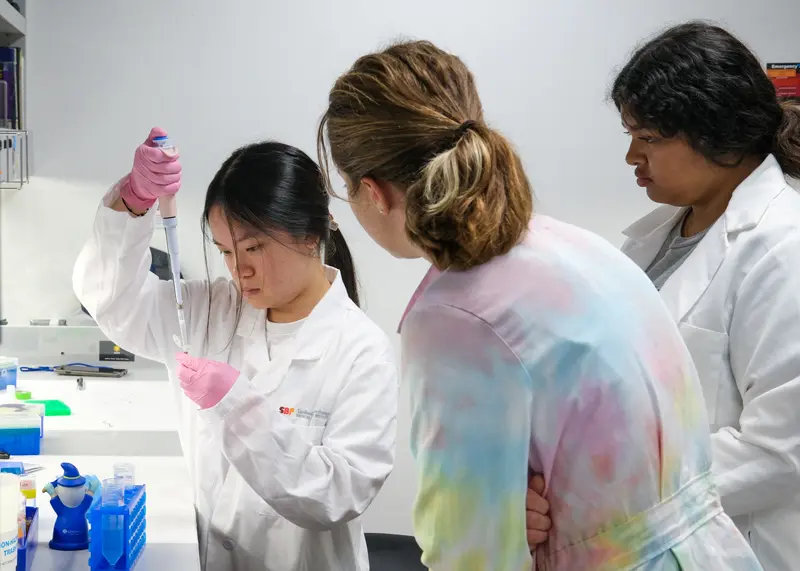
The series highlights the groundbreaking work and unique perspectives of women leaders in the biomedical sciences
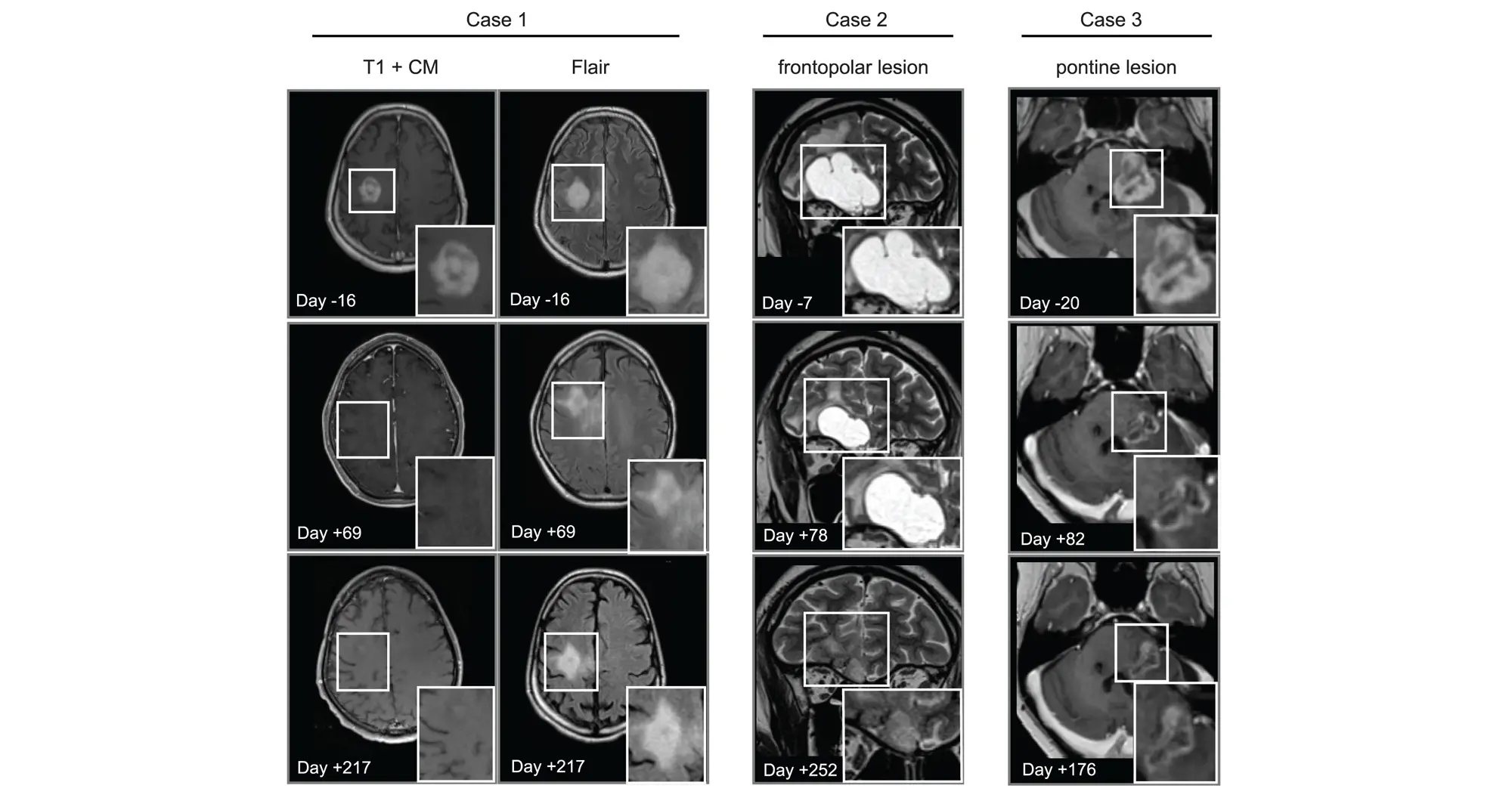
Susan Tousi, MBA, CEO at DELFI Diagnostics, opened the event by discussing the lessons she learned throughout her career journey. At DELFI Diagnostics, she is leading a team focused on improving the detection of lung cancer. The company’s goal is to make lung cancer screening more accessible through a blood test that is analyzed by applying machine learning and next-generation sequencing.
Prior to this role, Tousi served as a senior vice president for more than 10 years at Illumina, Inc., including as chief commercial officer for three years. During her tenure, she contributed to making genomic sequencing more affordable as the cost of sequencing a single genome fell from more than $5000 in 2013 to $200 in 2023. Tousi also borrowed from her experience developing consumer printers for Eastman Kodak and Hewlett-Packard, emphasizing the importance of making Illumina’s sequencing machines easy to use for clients in research labs, hospitals and clinics.
“My time at Illumina was amazing,” said Tousi. “I had the absolute privilege of seeing our genomic capabilities installed in 155 countries around the world.”
Tousi concluded with her optimism about how technology is transforming healthcare.
“I think we are on the precipice of major shifts in technology with the advancement of AI and where we’ve come with genomics, multiomics and the access to large-scale molecular data,” said Tousi. “I think you know these new technologies like blood-based liquid biopsy testing are going to allow us to find disease earlier, to treat it more precisely and monitor its recurrence across many disease areas.
“This can be the dawn of a new beginning in science and the advancement of healthy lives.”

From left: Brooke Emerling, PhD, and Susan Tousi, MBA
Image credit: Sanford Burnham Prebys
Kevin Tharp, PhD, assistant professor in the Cancer Metabolism and Microenvironment Program at Sanford Burnham Prebys, then moderated a fireside chat and audience question-and-answer session with Tousi and Brooke Emerling, PhD, director and associate professor in the Cancer Metabolism and Microenvironment Program. Topics included: different gender-based expectations in scientific fields; the importance of mentorship and paying it forward; dealing with the emotional toll of studying diseases more prevalent in women; and programs providing opportunities for future leaders in science and medicine.
The Women in Science Lecture Series features quarterly events and is part of broader efforts at Sanford Burnham Prebys to foster an environment that nurtures the success of individuals from all backgrounds. The series is hosted by the Office of Workforce Engagement & Belonging and highlights the groundbreaking work and unique perspectives of women leaders in the biomedical sciences, while fostering mentorship and collaboration across the Torrey Pines Mesa.
Women in Science lectures are free and open to the public. Registration is open for the next event in the series on February 11, 2026.