“I liked how hands-on everything was,” says Preuss intern Amayrani Calderon “The scientists would show us how to do the experiment but then let us do it ourselves. I’d never had that type of experience in a lab before.”
Each year, Sanford Burnham Prebys welcomes a cohort of high school interns from the Preuss School, whose students strive to be the first in their family to graduate from college. This year’s Preuss interns learned hands-on research skills from scientists at the Institute’s NCI-designated Cancer Center and about career possibilities in STEM beyond research.
“My favorite part of the program and about Sanford Burnham Prebys is all the diverse people I met,” says Alejandra Ruiz Ramirez, who is first-generation Mexican American. “I had mentally prepared myself not to see any scientists that look like me, or to potentially be stereotyped as a Mexican American woman, but that isn’t what happened at all. Everybody I met was very welcoming.”
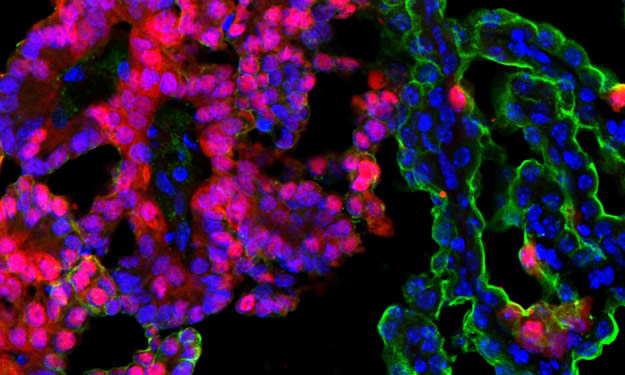
The Preuss internship is an intensive three-week program designed to jumpstart the careers of the next generation of scientific researchers. This year, the first two weeks were spent learning state-of-the art research techniques, such as staining cells for immunohistochemistry and separating proteins with gel electrophoresis.
“Seeing a real lab was a lot different than what I expected,” says Preuss intern Mohamed Haghi-Mohamed. “At school we just do labs on our desks, but seeing the incubators and other machines really changed my perspective and on how science works in the real world.”
For the final week of the program, interns shadowed staff scientists working in various labs throughout the Cancer Center, where they saw the research process firsthand.
“Consuming a lot of media makes you see science as always exciting and fast-paced, but it’s a very different experience actually working in the lab day to day,” says Preuss intern Juan Lomas Hoeung. “Sometimes there’s a lot of downtime but other times things are hectic.
The Preuss internship program also included activities outside of the lab, including panel discussions with scientists, a tour of the Conrad Prebys Center for Chemical Genomics, and a workshop on diversity and equity and STEM. The interns also had lunch with Institute staff each day, where they had the chance to learn and ask questions about varied STEM careers such as research administration, science communication, and philanthropy.
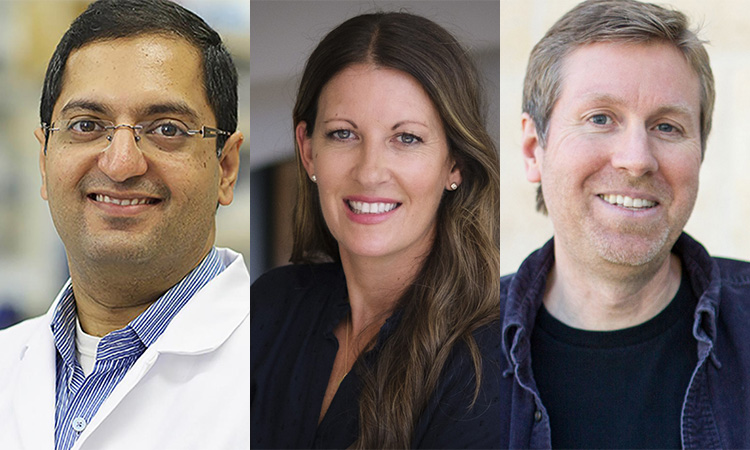
“We wanted the students to see that there are varied paths to a career in STEM, and that these paths aren’t always linear,” says Victoria Carrillo, senior program administrator for the Cancer Center, who oversaw the Preuss internship along with faculty organizer Svasti Haricharan, PhD.
The program culminated in a celebratory luncheon with students, researchers and Institute staff, where the interns had the opportunity to share what they’ve learned from their experience at Sanford Burnham Prebys.
“This was the best environment to learn in because the people here are some of the most expressive and passionate people I’ve met when they’re in the lab talking about what they do,” says Hoeung. “Everybody was so enthusiastic.”