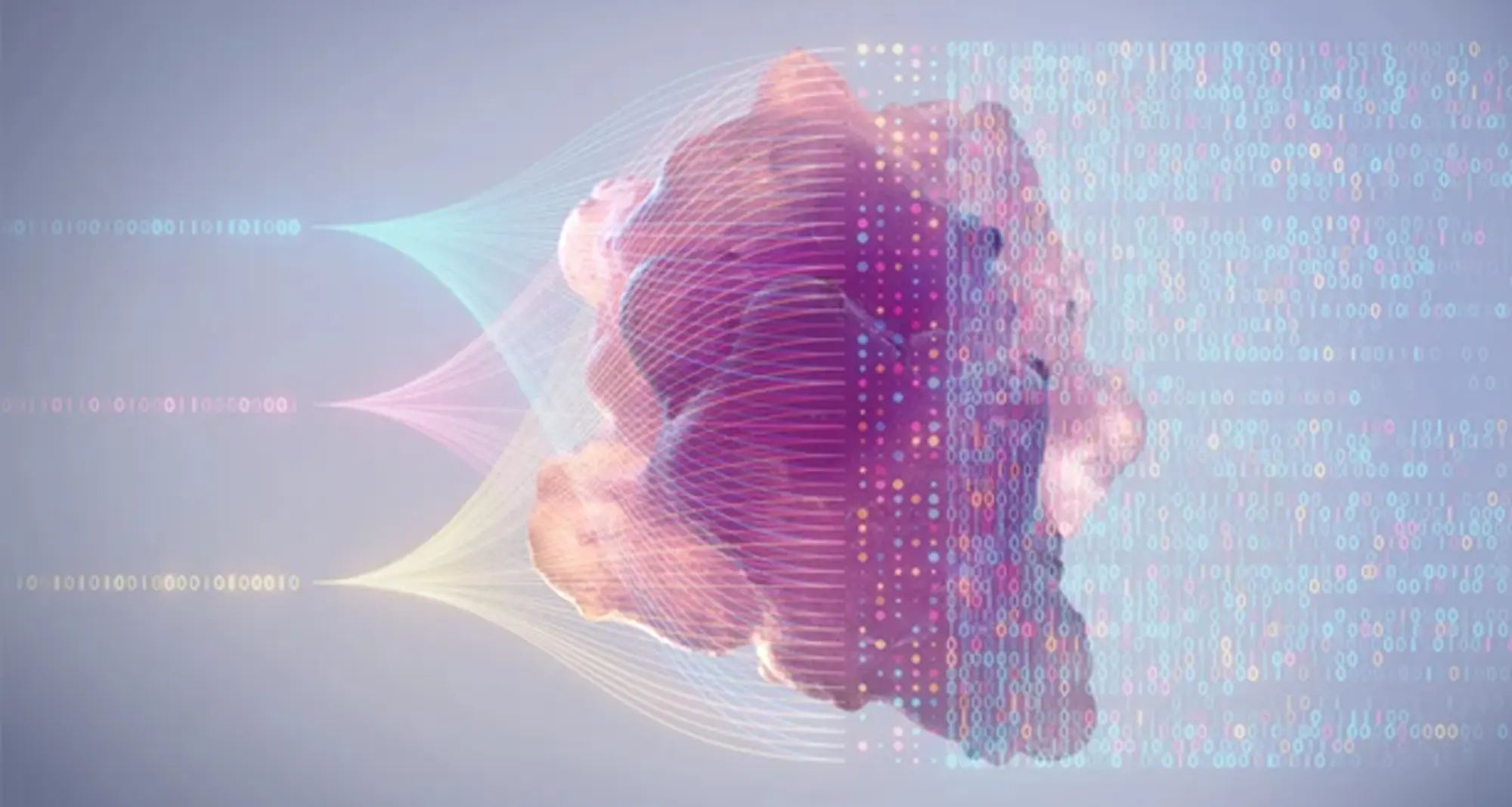
PERCEPTION is the acronym for PERsonalized Single-Cell Expression-Based Planning for Treatments In Oncology, an artificial intelligence-based tool that, in findings first reported last year, was able to predict tumor response to targeted therapy using single-cell datasets.
The work, published in Nature Cancer, is the result of first study author Sanju Sinha, PhD, assistant professor in the Cancer Metabolism and Microenvironment Program at Sanford Burnham Prebys, with senior authors Eytan Ruppin, MD, PhD, and Alejandro Schaffer, PhD, at the National Cancer Institute (NCI), part of the National Institutes of Health, and colleagues.
Recently, the NCI’s Center for Cancer Research highlighted PERCEPTION in its 2024-2025 annual Milestones report.
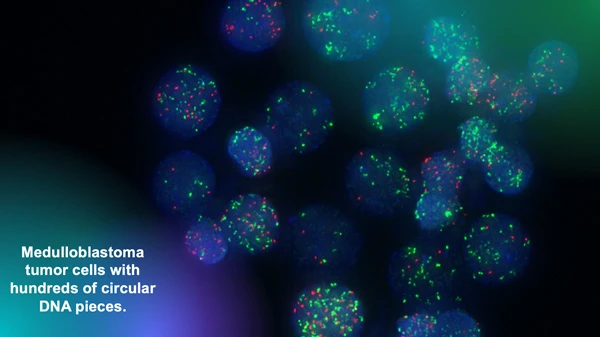
The researchers said PERCEPTION not only helped predict which anti-cancer drugs are most effective for individual patients, but also tracked the evolution of drug resistance over the course of the disease and treatment — something never before achieved.
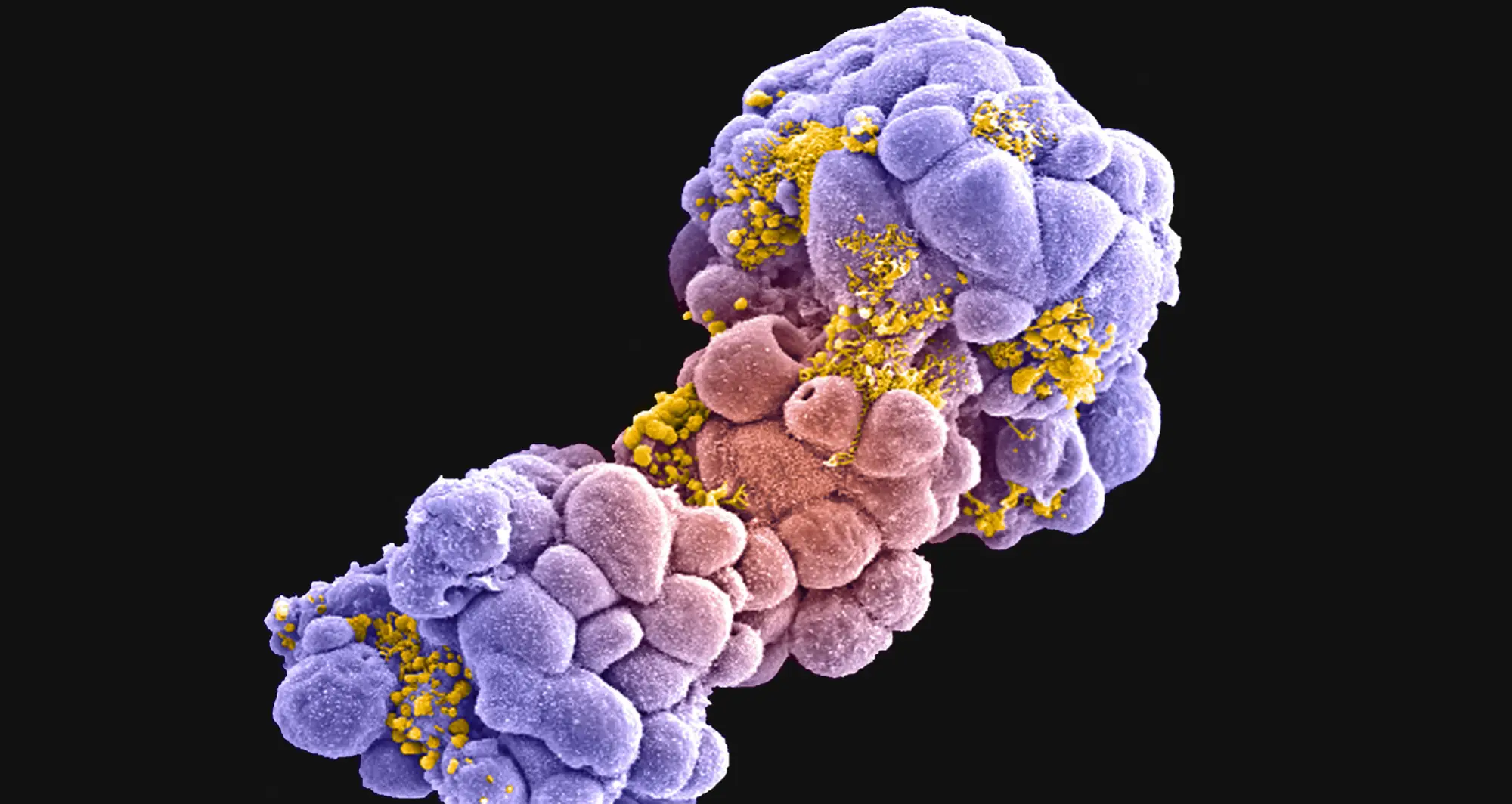
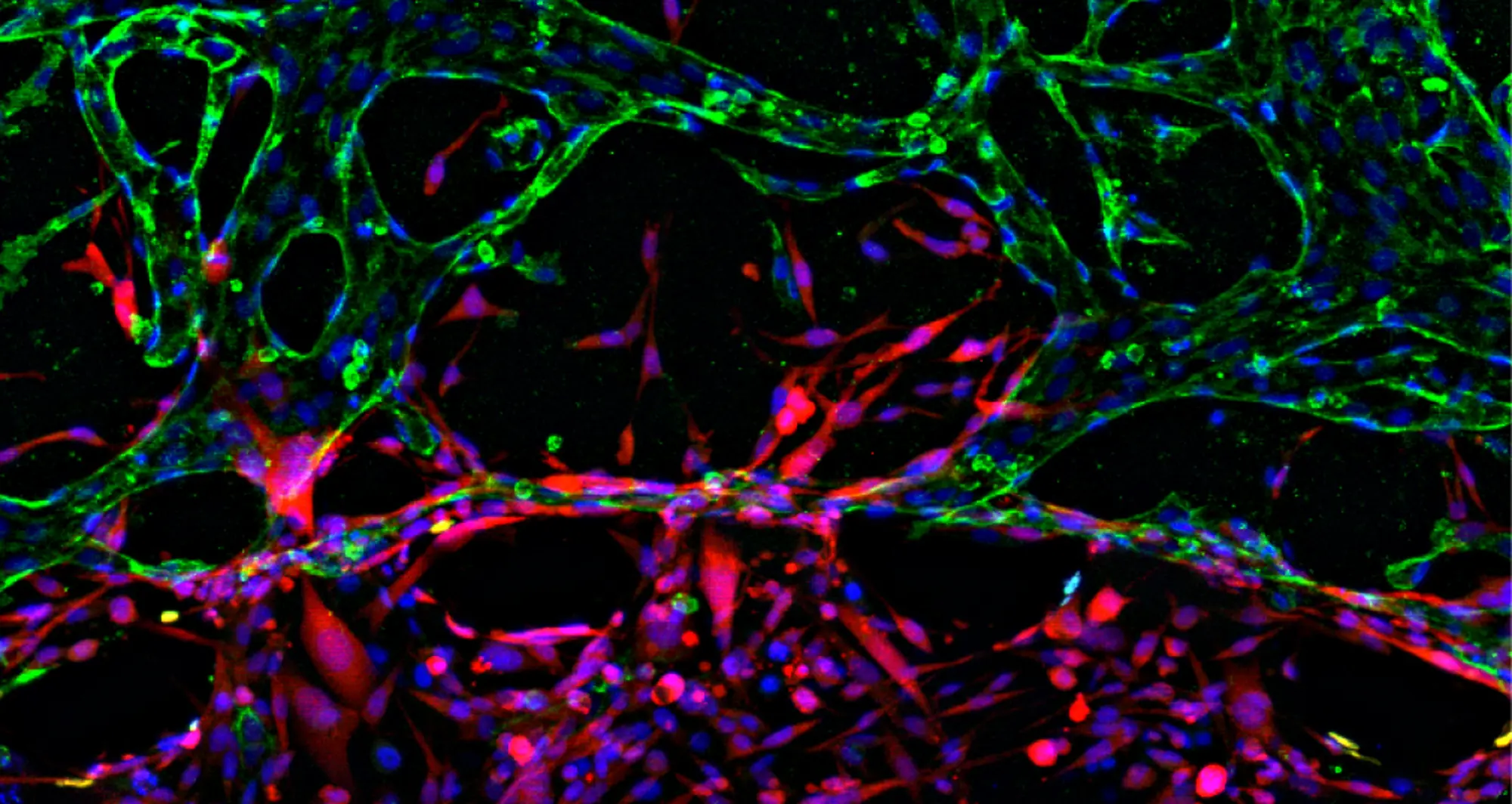
“A tumor is a complex and evolving beast. Using single-cell resolution can allow us to tackle both of these challenges, Sinha said when their findings were published. “PERCEPTION allows for the use of rich information within single-cell omics to understand the clonal architecture of the tumor and monitor the emergence of resistance.” (In biology, omics refers to the sum of constituents within a cell.)
“The ability to monitor the emergence of resistance is the most exciting part for me. It has the potential to allow us to adapt to the evolution of cancer cells and even modify our treatment strategy.”
PERCEPTION was previously named among the National Institutes of Health director’s highlights for 2024.