The October Science Connect Series event was themed around Breast Cancer Awareness Month and featured two cancer research experts.
The Sanford Burnham Prebys Wellness Ambassadors hosted a Science Connect event on Wednesday, October 30, 2024, featuring two faculty experts discussing their breast cancer research and its implications.
The Science Connect Series provides a forum for Sanford Burnham Prebys principal investigators to share their research with administrative personnel. Faculty members gain experience in communicating their science to a lay audience, and administrators gain a better understanding of research conducted at the institute so they can become better advocates and ambassadors of the shared mission to translate science into health.
Kelly Kersten, PhD, an assistant professor in the Cancer Metabolism and Microenvironment Program, opened the event by focusing on the importance of finding new treatments —such as immunotherapies — for the one-third of breast cancer patients that are diagnosed after the early stages of the disease when surgery is less effective.
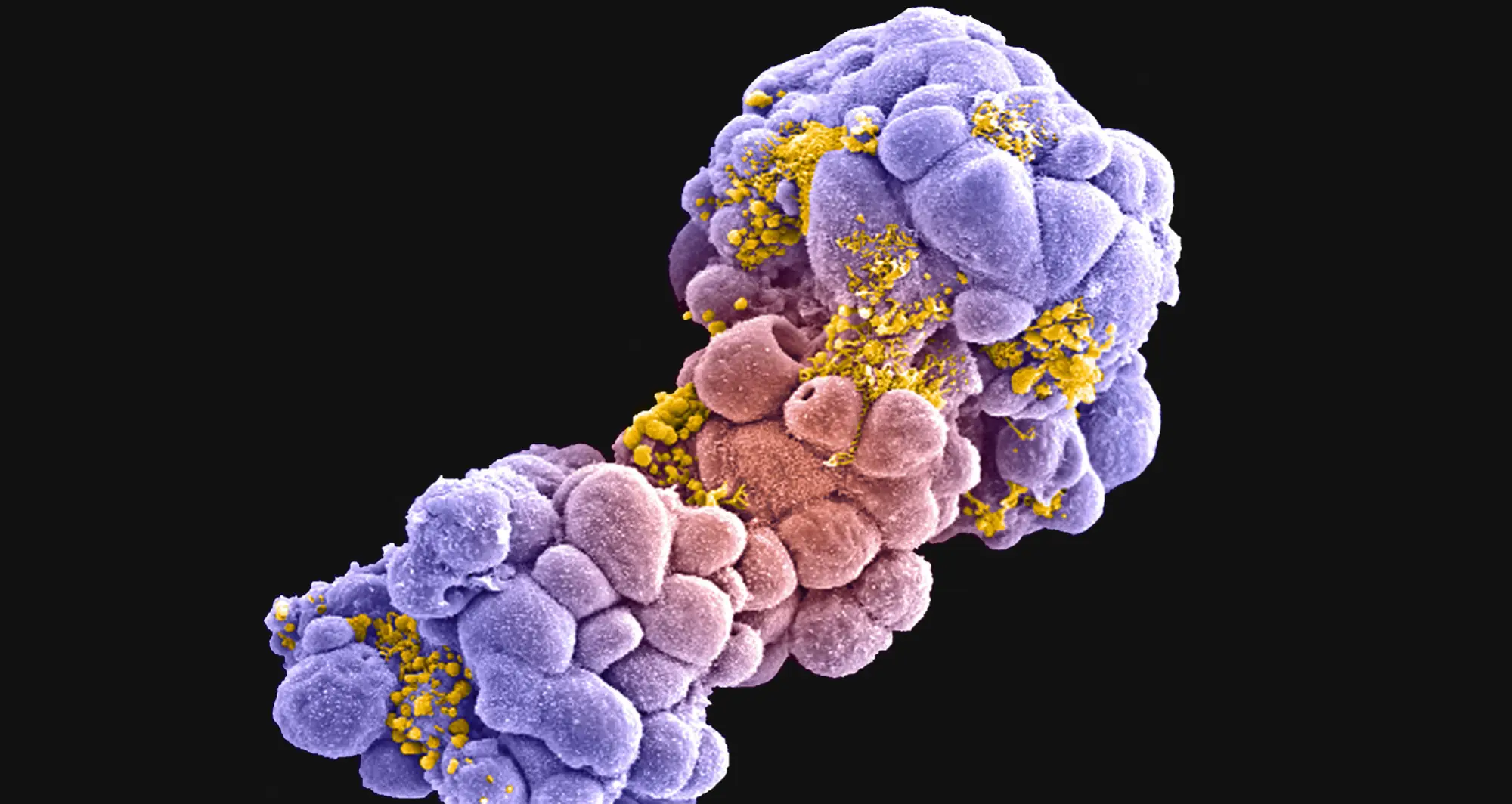
The immune system is one of the main defenses of the human body to fend off harmful pathogens and invasive cells, such as cancer. Among all white blood cells, a particular cell type, called a T cell, can directly kill cancer cells and therefore plays an essential role in building anti-tumor immune responses.
Many types of cancer are confronted and infiltrated by T cells, only to be suppressed by the local tumor environment.
“While immunotherapies that boost the immune system have revolutionized the way we treat cancer, many patients do not respond to the treatments, and the mechanisms of resistance remain largely unclear,” said Kersten.
Kersten’s goal is to understand why T cells enter a state known as exhaustion and lose their tumor-killing capacity. This knowledge will help her team find potential future therapies that could prevent T-cell exhaustion and improve immunotherapies for cancer patients.
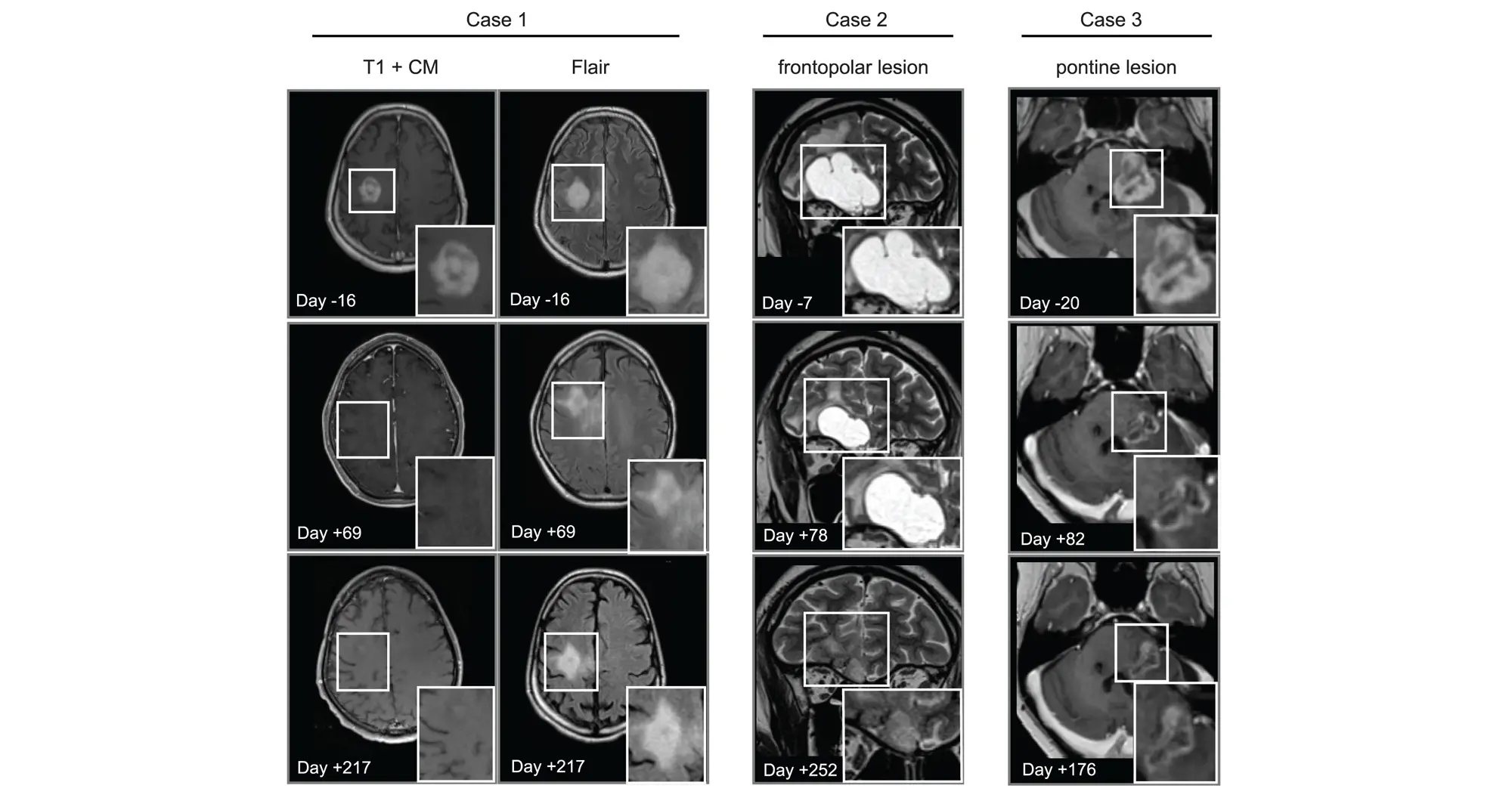
Kevin Tharp, PhD, also an assistant professor in the Cancer Metabolism and Microenvironment Program, shared that his lab’s focus is on how cancer cells adapt their metabolism to generate the energy needed to spread to other tissues through metastasis. He presented his team’s work with the Kersten lab on another aspect of potential resistance to immunotherapy in breast cancer.
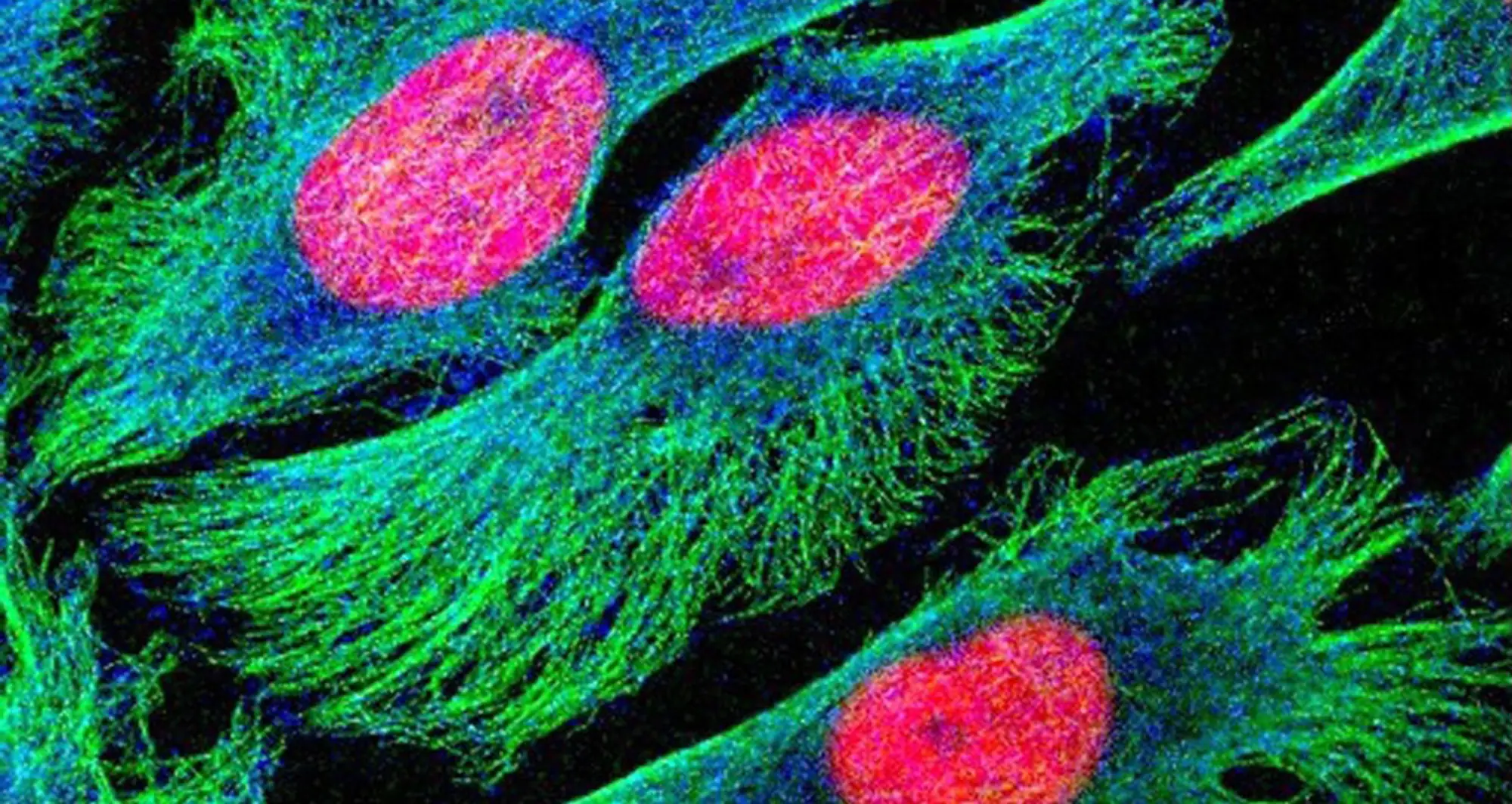
Tharp and Kersten are studying the hypothesis that part of the reason why these therapies fail is due to tumor-associated fibrosis, the creation of a thick layer of fibrous collagen (like scar tissue) that acts as a barrier against the anti-tumor immune response. They published a paper on June 3, 2024, in Nature Cancer, discussing how tumor-associated macrophages, a type of immune cell found abundantly in the tumor microenvironment, respond to the physical properties of fibrosis.
By synthesizing injury-associated collagens that facilitate wound closure, TAMs experience metabolic changes and generate metabolic byproducts that suppress the anti-tumor function of immune cells.
“The metabolic changes in the microenvironment present more of a challenge to anti-tumor responses than the physical barrier,” said Tharp. “Our study provides an alternative explanation for why anti-tumor immunity is impaired in fibrotic solid tumors.”
To follow up on these results, Tharp is collaborating with Sarah Blair, MD, a professor of surgery at the University of California San Diego, to fund and initiate a clinical trial testing the potential of dietary supplements to counteract the suppressive effects of TAM metabolic byproducts as an adjunct therapy to surgery.