The four-day event included talks from experts from across North America and opportunities to discuss improving experimental methods and approaches to analyzing the resulting data.
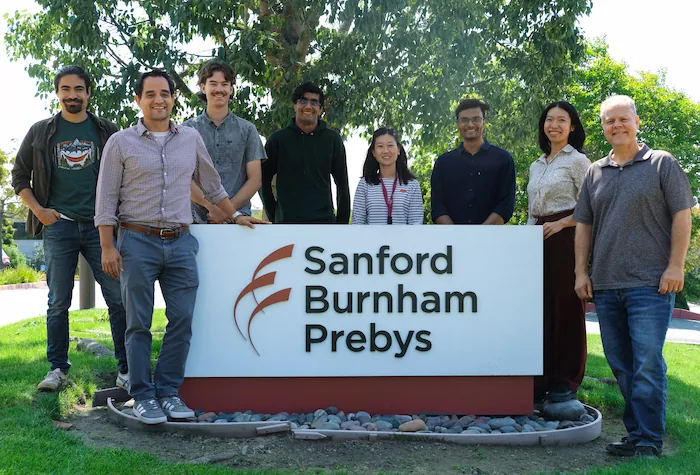
Researchers convened at Sanford Burnham Prebys in La Jolla from September 12-15 to hear presentations from their peers and confer about the latest developments in modifying the genomes of mammalian animal models to advance biomedical research.
Anindya Bagchi, PhD, associate professor in the Institute’s Cancer Genome and Epigenetics Program, planned the 4th Mammalian Genome Engineering Symposium, which included 26 presentations from experts across the United States and Canada. Attendees asked many questions throughout, and numerous speakers commented on how valuable the conversation at the meeting was for refining planned experiments and considering new ideas and approaches.
“It was a truly enjoyable and thought-provoking meeting,” said Angela Liou, MD, an instructor in the Cancer Genome and Epigenetics Program at Sanford Burnham Prebys and pediatric oncologist and hematologist at Rady Children’s Hospital-San Diego. “It also was incredibly helpful in informing the next steps of my research project.”
“I’m so grateful for the invitation to attend this symposium,” said Praveen Raju, MD, PhD, the Nathan Gordon Chair in Neuro-Oncology and medical director of the Pediatric Neuro-Oncology Program at Rady Children’s Hospital-San Diego and director of the Pediatric Neuro-Oncology Program at the University of California San Diego School of Medicine.
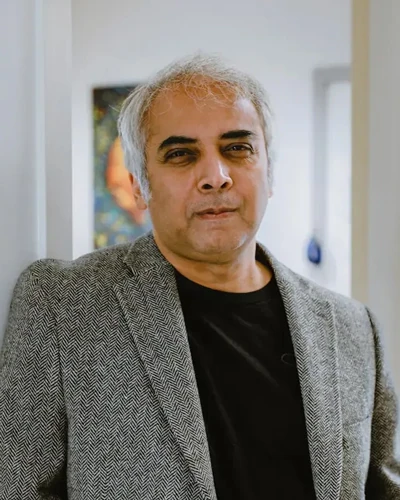
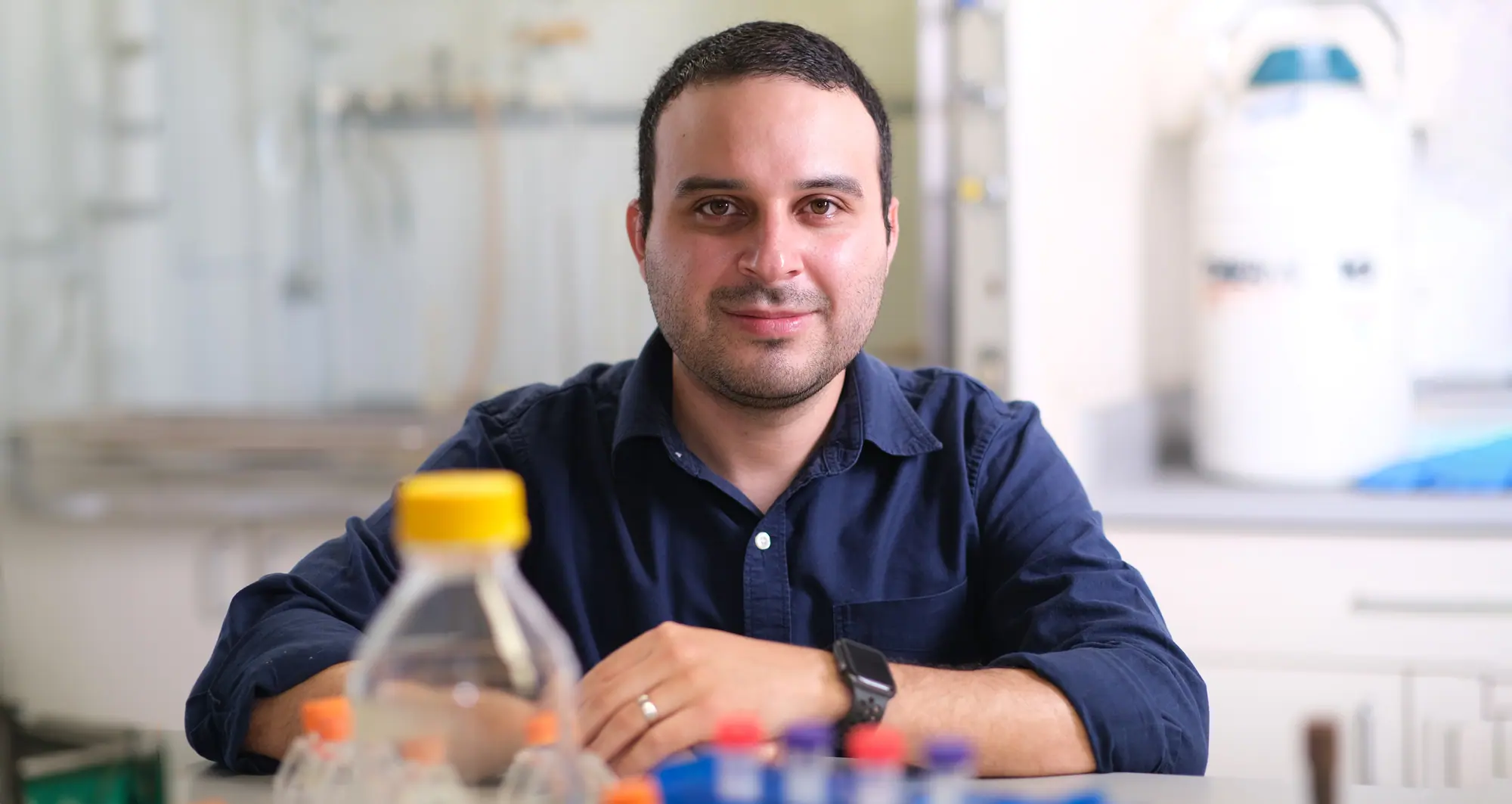
Anindya Bagchi, PhD, is an associate professor in the Cancer Genome and Epigenetics Program.
“The presenters and attendees were welcoming and collaborative, and I certainly learned a lot.”
The symposium brings together the Mammalian Genome Engineering Group, which was formed by a small group of genome engineering enthusiasts including Bagchi, Nada Jabado, MD, PhD, professor of Pediatrics and Human Genetics at McGill University and a hematologist and oncologist at Montreal Children’s Hospital; David Largaespada, PhD, a professor of Pediatrics, Genetics, Cell Biology and Development at the University of Minnesota Medical School and the associate director for Basic Research in the Masonic Cancer Center; and Michael Taylor, MD, PhD, The Cyvia and Melvyn Wolff Chair of Pediatric Neuro-Oncology at Texas Children’s Cancer and Hematology Center and professor of Pediatrics (Hematology-Oncology) at Baylor College of Medicine.
The group is interested in developing functional models of genomic and epigenetic mutations associated with human diseases—especially cancers—that are difficult to recreate in animal models. The group’s first symposium was coordinated by Taylor in Napa, Calif., in 2014, followed by the 2nd symposium that was organized by Jabado in Montreal in 2015. After a hiatus, the group was revived in 2023 with the 3rd symposium hosted again by Taylor in Houston.
“We believe this symposium will, in the coming years, become a leading forum for discussing cutting-edge genomic and epigenomic approaches to tackle challenging genetic and epigenetic mutations,” said Bagchi. “These approaches are likely to become standard practice in the near future.”
The Sanford Burnham Prebys scientists that presented at the 4th Mammalian Genome Engineering Symposium were:
- Bagchi, “Why are MYC-driven cancers so lethal?”
- Liou, “Investigating the deposition of H3.3K27M oncohistone and its effect on retrotransposon reactivation in H3K27M pediatric diffuse midline glioma”
- Ani Deshpande, PhD, associate professor in the Cancer Genome and Epigenetics Program and associate director of Diversity, Equity and Inclusion in the NCI-Designated Cancer Center, “Functional genomic approaches to identify selective dependencies in synovial sarcoma”
- Peter D. Adams, PhD, the director of the Cancer Genome and Epigenetics Program, “The role of aging in cancer”
- Lukas Chavez, PhD, associate professor in the Cancer Genome and Epigenetics Program, “Circular extrachromosomal DNA promotes tumor heterogeneity and enhancer rewiring”
- Jerold Chun, MD, PhD, professor in the Degenerative Diseases Program, “Genetic mosaicism and somatic gene recombination in the brain”
- Adarsh Rajesh, graduate student, Sanford Burnham Prebys, “CCND1-CDK6 complex inhibits DNA damage repair and promotes inflammation in senescence and the aged liver”
Additional speakers included:
- Taylor, “Why does medulloblastoma love to be tetraploid and other nonsense”
- Jabado, “Co-opting 3D structures to fuel tumorigenesis”
- Tannishtha Reya, PhD, Herbert and Florence Irving Professor of Basic Science Research in Physiology and Cellular Biophysics, Columbia University, “New genetically engineered models to understand cancer heterogeneity and therapy resistance in pancreatic cancer”
- Simona Dalin, PhD, postdoctoral fellow, Broad Institute of the Massachusetts Institute of Technology and Harvard University, “Contributions of perfect and imperfect homology to rearrangement formation in human and cancer genomes”
- Alison M. Taylor, PhD, assistant professor of Pathology and Cell Biology, Columbia University, “Functional and computational approaches to uncover the consequences of chromosome arm aneuploidy in cancer”
- Sean Eagan, PhD, senior scientist in the Cell Biology program at The Hospital for Sick Children, professor of Molecular Genetics, University of Toronto, “An update on Genetic analysis of 16q-syntenic block deletion in the mouse mammary gland – a tumor suppressor arm”
- Claudia Kleinman, PhD, associate professor of Human Genetics, McGill University, investigator at the Lady Davis Institute for Medical Research, Jewish General Hospital, “Lineage programs and the 3D genome in pediatric brain tumors”
- Branden Moriarity, PhD, associate professor of Pediatrics (Hematology and Oncology), University of Minnesota Medical School, “Next generation engineered immune effector cells for immunotherapy”
- Beau Webber, PhD, associate professor of Pediatrics (Hematology and Oncology), University of Minnesota Medical School, “Building cancer in a dish: Sarcoma modeling using human pluripotent stem cells”
- Sameer Agnihotri, PhD, associate professor of Neurological Surgery and director of the Brain Tumor Biology and Therapy Lab, University of Pittsburgh Medical Center Children’s Hospital of Pittsburgh, “Identifying genetic vulnerabilities by modeling Chromosome 9p loss”
- Largaespada, “Loss of the polycomb repressor complex 2 (PRC2) alters the super-enhancer landscape, genome/epigenome stability, and therapeutic sensitivities of malignant peripheral nerve sheath tumors”
- Teresa Davoli, PhD, assistant professor of Biochemistry and Molecular Pharmacology, New York University Langone Health, “Engineering chromosome specific aneuploidy by targeting human centromeres”
- Rameen Beroukhim, MD, PhD, associate professor of Medicine, Dana-Farber Cancer Institute and Harvard Medical School, associate member of the Broad Institute of MIT and Harvard, “Detecting rearrangement signatures—naturally”
- Quang Trinh, PhD, scientist, Ontario Institute for Cancer Research, “Perspectives and Challenges in PFA Integrative Analysis”
- Taylor Gatesman, graduate student, University of Pittsburgh, “Genome Engineering: DREaming of and vCREating new models”
- Joseph Skeate, PhD, postdoctoral fellow, University of Minnesota Medical School, “Targeted CAR integration and multiplex base editing in a single-step manufacturing process for enhanced cancer immunotherapies”