Lynne Selinka knew in her heart that something was seriously wrong with her 10-year-old son, Travis. For months he had experienced dizziness, vomiting and headaches, despite his doctor’s best efforts to find a cause. A visit to Rady Children’s Hospital-San Diego revealed a heartbreaking diagnosis: Travis had a malignant brain tumor. He was operated on the next day and then endured two months of radiation treatment followed by six rounds of chemotherapy.
“That year, Travis asked Santa, ‘Can I please be done with chemo before Christmas?’” Lynne said. “It was by far the hardest year of our life.”
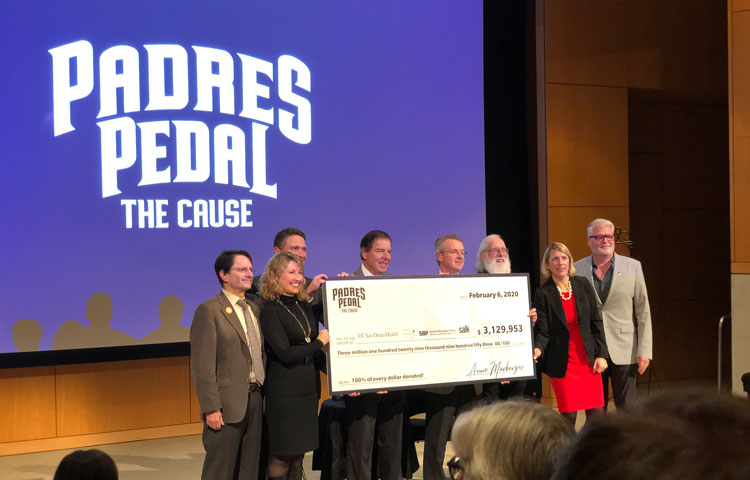
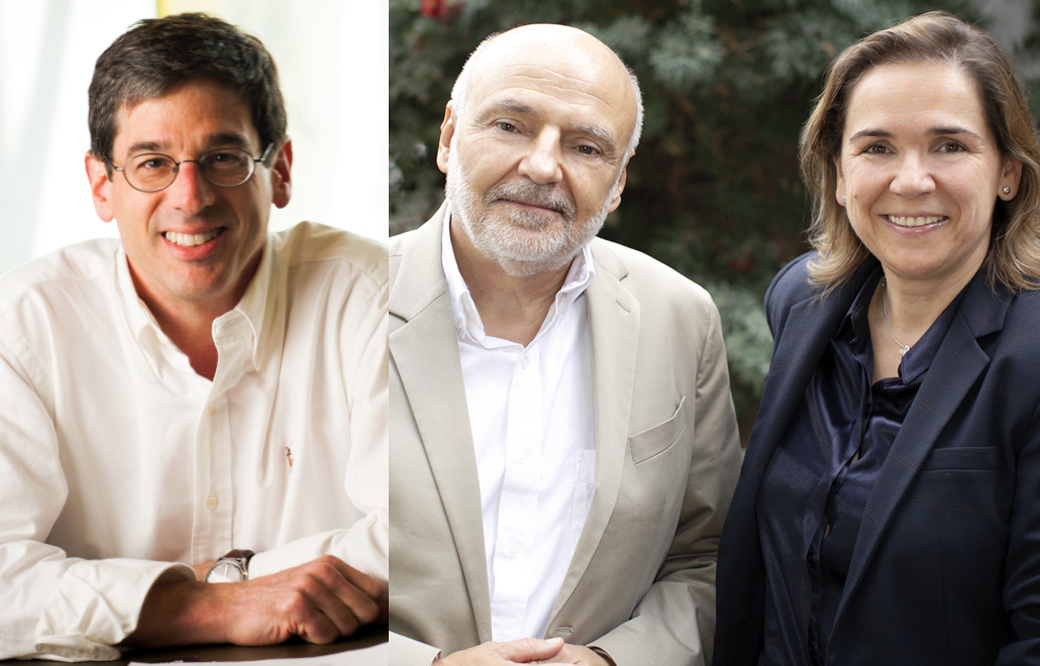
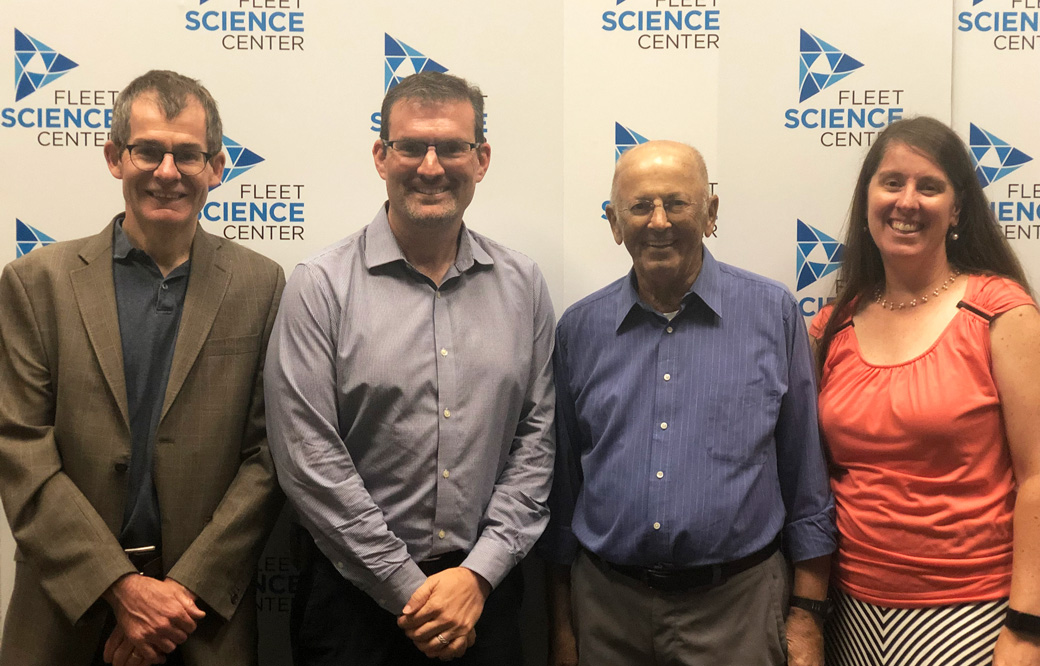
Brain tumors are the most common cause of cancer-related death in children—recently surpassing leukemia. To help the public learn about the latest efforts to develop better treatments for pediatric brain cancer, our Institute teamed up with the Fleet Science Center to host a panel discussion on Sunday, December 8. Travis and his parents, Lynne and Tony, shared their story alongside the clinician who treated Travis, John Crawford, MD, director of Pediatric Neuro-Oncology at Rady Children’s Hospital-San Diego; and a scientist working on personalized treatments for pediatric brain cancer, Robert Wechsler-Reya, PhD, of Sanford Burnham Prebys and Rady Children’s Institute for Genomic Medicine.
As the speakers explained, while aggressive therapies have improved outcomes for children with brain tumors (today Travis is a junior in high school), one in four children with a malignant brain tumor does not survive. Children who do survive have an increased risk of severe long-term side effects from undergoing aggressive treatment at such a young age, including developing additional cancers or experiencing intellectual disability. Six years after he was declared cancer-free, Travis was diagnosed with chronic myeloid leukemia, a type of blood cancer caused by his previous chemotherapy. So far, his new treatment is working.
Wechsler-Reya hopes his work to develop personalized therapies based upon an individual’s tumor could help spare children from this painful experience. By analyzing patient tumor samples—obtained from Rady Children’s Hospital—his team works to understand the cancer at a molecular level, studying the tumor’s DNA mutations, changes in gene expression, responses to drugs, and much more. Armed with this information, the scientists then work to find therapies that are customized to a child’s specific tumor—and may be more effective and less toxic.
“For pediatric brain cancer, success doesn’t just mean better treatments. It also means developing treatments with fewer long-term side effects,” says Wechsler-Reya. “If successful, this work might help more children not only survive brain cancer, but also live a long, healthy life after treatment.
Travis and his family welcome this work with open arms.
“We try to look for a silver lining in every day. Travis has become an amazing public speaker and now shares his story with other children fighting brain cancer. But each part of our journey has been so hard—from receiving the diagnosis, seeing Travis go through a painful surgery and then chemo, not knowing if the treatments would work, and then being diagnosed with another cancer almost six years later,” said Lynne. “We are so grateful for the efforts of researchers who are working toward a world where a child doesn’t have to go through what Travis did—or at least is spared from some of the hardest parts of the journey.”
This event was the last of our five-part “Cornering Cancer” series at the Fleet Science Center. Read about our past discussions focusing on lung, blood, breast and pancreatic cancers.