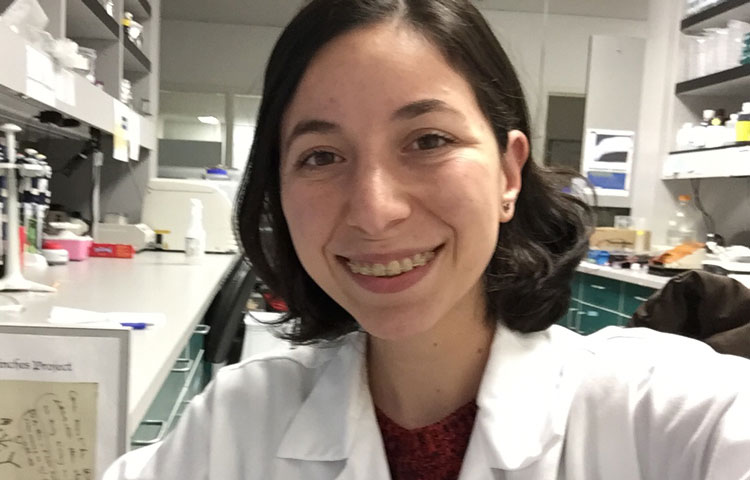
Barbosa Guerra is working to find better treatments for a deadly leukemia
For Karina Barbosa Guerra, touring a lab and meeting scientists as part of her Girl Guides troop—Mexico’s equivalent of the Girl Scouts—was a life-changing experience. Suddenly, she could see herself as a scientist.
Today, Barbosa Guerra is a graduate student in the Deshpande lab at Sanford Burnham Prebys, where she’s working to find better treatments for a blood cancer called acute myeloid leukemia (AML). We caught up with Barbosa Guerra as she prepares to take the virtual stage at the Diversity and Science Lecture Series at UC San Diego (DASL) to learn more about when she decided she wanted to be a scientist and where she can be found when not in the lab.
Tell us about the moment you realized you wanted to be a scientist.
According to my mother, I stated that I wanted to become a chemist to develop vaccines when I was ten years old. However, it wasn’t until middle school that I started cultivating my own sense of scientific curiosity. At that time, I was in a Girl Scouts program centered on HIV/AIDS peer education, so I began to read a bit more about viruses. It was incredibly amazing that they could linger undetected in our bodies—and that many questions about their biology remained unanswered. The more I learned, the less I felt I knew, and I wanted to follow that endless string of questions.
What do you study, and what is your greatest hope for your research?
I study a cancer called acute myeloid leukemia—specifically, subtypes that are hard to treat. Certain cancer cells, like stem cells, are pretty resilient and can self-renew. This enables them to resist therapy, so we want to discover better ways to target this particular feature. My research aims to find ways in which we can treat these leukemias based on their stem cell–like capabilities. My hope is that we can ultimately benefit the patients enduring harsh treatments and disease relapse, and along the way, illuminate the fascinating aspects of the biology behind effective treatments.
What do you wish people knew about science?
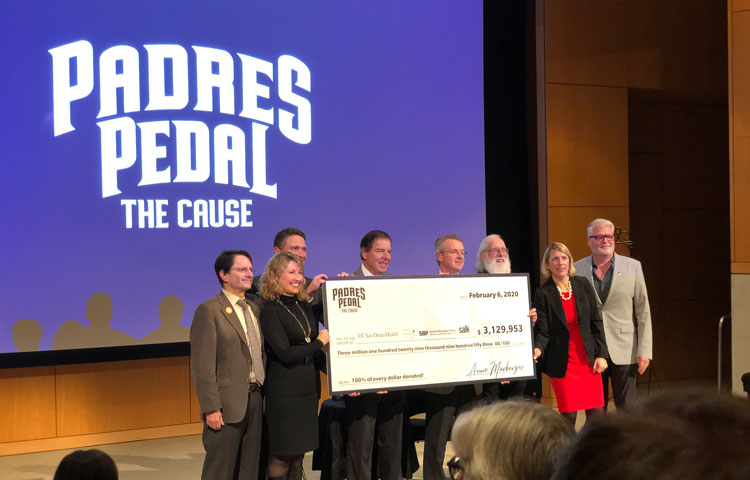
That it’s a team effort. The current coronavirus pandemic has really shown us that collaboration is at the heart of transformative science. I think that great ideas are best developed through discussion—and the thrill of putting the pieces together is way more enjoyable with company.
How do you think your lab colleagues would describe you?
Maybe as the girl with a bunch of notebooks. I like to make notes of everything. My notebooks are way more reliable than my memory.
What is the best career advice you’ve ever received?
Early in the graduate program, one of my mentors told me, “Be there,” meaning that I had to spend time with my science. If I were to discover something or make a great insight, I had to be there to do it, think it or see it.
What do you wish people knew about Sanford Burnham Prebys?
That this is such a welcoming community. I felt this the very first time I visited the campus, and I feel so at home here as a student. There are plenty of opportunities to engage with others and help each other out. I really enjoy the collaborative spirit of our little community.
Learn more about the Institute’s Graduate School of Biomedical Sciences.