The San Diego-based philanthropic organization has awarded $43 million in cancer research to date
Curebound recently announced the awarding of 17 grants in December 2024 for a total of $8.25 million in funding to advance cancer research in 2024.
Two new grants will support cancer research conducted by scientists at Sanford Burnham Prebys. Since 2014, 32 Curebound grants have supported projects that included scientists at the institute.
A workaround for a tricky target
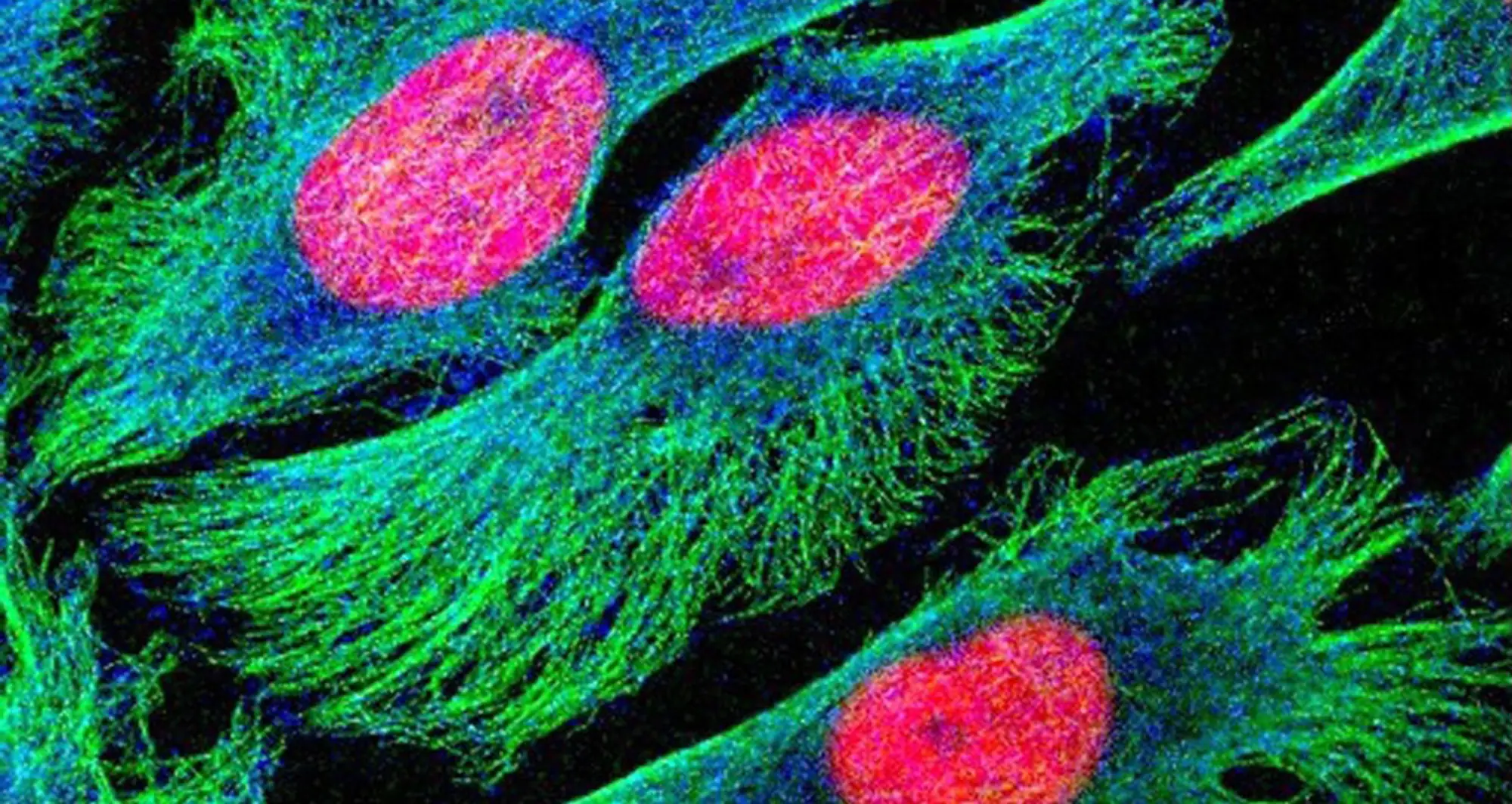
The TP53 gene contains the blueprint for constructing a protein called tumor protein p53. This protein is considered a tumor suppressor because it helps cells grow in a controlled manner.
When cell growth goes awry, however, the TP53 gene is a common culprit as the most frequently mutated gene in cancers. While this ubiquity has placed a bullseye on the mutated tumor protein p53 for aspiring drug developers, it has proven tricky to target directly.
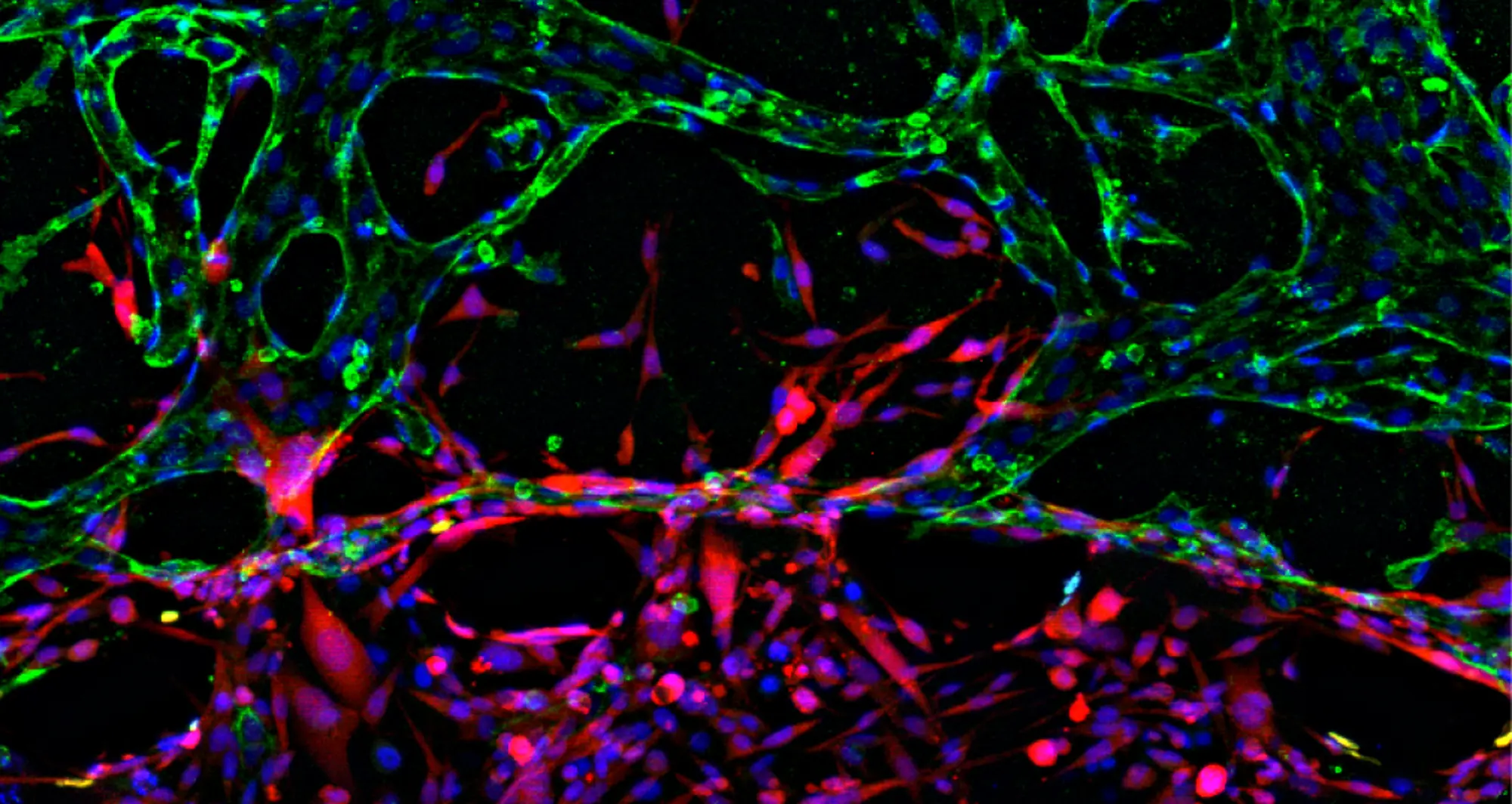
Brooke Emerling, PhD, director of the Cancer Metabolism and Microenvironment Program, and her collaborators have shown that the growth of cancer cells with a mutated TP53 gene is dependent on lipid enzymes called phosphatidylinositol-5-phosphate 4-kinases (PI5P4K). Emerling and her collaborators have identified compounds that break down these enzymes.
The researchers have demonstrated the ability of these compounds to target and eliminate cancer cells with a mutated TP53 gene without harming normal cells. Curebound will support the team’s ongoing efforts to work around the difficult-to-target tumor protein p53 by instead targeting PI5P4K.
Next, the group plans to optimize the compounds that break down PI5P4K to develop cancer drugs that are strong candidates for future clinical trials.
Curebound collaborators: Patrick Kearney, PhD, director of Medicinal Chemistry in the Conrad Prebys Center for Chemical Genomics, and Eric Wang, PhD, assistant professor in the Cancer Molecular Therapeutics Program.
Boosting the immune system against lung cancer
The immune system is one of the main defenses of the human body to fend off harmful pathogens and invasive cells such as cancer. Among all white blood cells, a particular cell type, called a T cell, can directly kill cancer cells and therefore plays an essential role in building anti-tumor immune responses.
Immunotherapies that boost the anti-cancer capabilities of T cells have revolutionized the way we treat cancer, especially in blood cancers such as leukemia, lymphoma and myeloma. More recently, immunotherapies are rapidly advancing to become mainstream treatments for solid cancers as well.
Currently, however, less than a third of patients with lung cancer benefit from immunotherapies. Pandurangan Vijayanand, MD, PhD, the William K. Bowes Distinguished Professor at the La Jolla Institute for Immunology, discovered that certain T cells called cytotoxic T lymphocytes have molecular features associated with a robust immune response against lung cancer tumors. His work has identified new targets for lung cancer immunotherapy.
Curebound will support Vijayanand’s collaboration with Michael Jackson, PhD, senior vice president for Drug Discovery and Development in the Conrad Prebys Center for Chemical Genomics, to use this research to identify agents to boost tumor immune responses.
The research team’s work has the potential to identify a new class of immunotherapy drugs for patients with lung cancer.
Curebound collaborator: Changlu Liu, PhD, director of Receptor Pharmacology in the Conrad Prebys Center for Chemical Genomics.

Pandurangan Vijayanand, MD, PhD, is the William K. Bowes Distinguished Professor at the La Jolla Institute for Immunology.